Arteriosclerosis: warning signals, dangers, treatment
Arteriosclerosis: warning signals, dangers, treatment
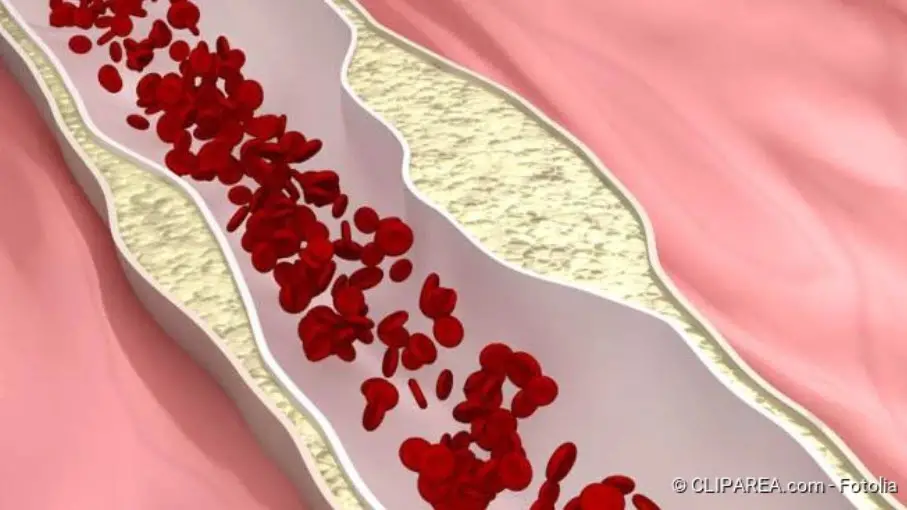
In the case of arteriosclerosis, the arteries become narrowed by deposits. As a result, the blood flow is restricted or, in the worst case, completely interrupted – then there is the threat of a heart attack. Older people are particularly often affected by arteriosclerosis, but lifestyle factors such as a high-fat diet or lack of exercise also increase the risk of arteriosclerosis. Here you can find out everything you need to know about risk factors, consequences and prevention of arteriosclerosis.
Arteriosclerosis: Description
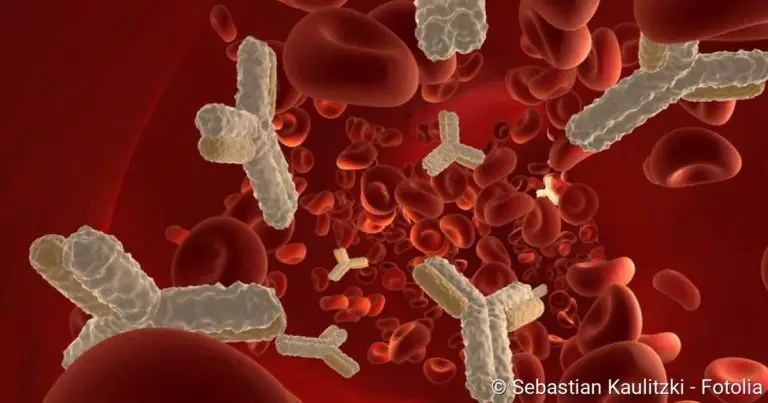
Arteriosclerosis, colloquially known as hardening of the arteries, is a disease of the arteries in the body (arteries). By definition, these blood vessels carry the blood away from the heart. In the large bloodstream they transport oxygen-rich blood from the heart to the organs, muscles and tissues. In arteriosclerosis patients, blood lipids, blood clots, connective tissue and calcium are deposited in the vessel walls. These deposits are called plaques.
Arteriosclerosis comprises all hardenings of the arterial wall. This also includes, for example, Mönckeberg mediasclerosis, in which the middle vessel wall (media) calcifies. It is the result of too much calcium in the blood and is associated with diseases such as chronic kidney failure or diabetes. The best-known and most common form of arteriosclerosis with plaque formation in the inner vessel wall (intima) is called atherosclerosis. In everyday language, however, the two terms are often used interchangeably.
In principle, arteriosclerosis can develop in all arteries of the body, but it preferentially develops in certain vascular regions in the neck, brain, heart, pelvis or the main and leg arteries. Particularly common are sites where the blood flow encounters obstacles due to physical factors – for example at vascular branches. The consequence of arteriosclerosis: the blood vessels become narrower and lose their elasticity.
This prevents the blood from flowing freely. In the worst case, a clot of blood platelets (thrombus) forms on the plaques – then a heart attack is imminent. However, arteriosclerosis can also weaken the vessel wall to such an extent that it expands and an aneurysm develops. Consequences of arteriosclerosis are the most frequent cause of death in western industrial nations.
Arteriosclerosis: symptoms
Arteriosclerosis develops slowly – often corresponding symptoms only appear after years or decades. Often, the symptoms of arteriosclerosis do not appear until older age. How the disease manifests itself depends on which vessels in the body are affected.
If the coronary vessels are narrowed, coronary heart disease is present. Symptoms are caused by reduced blood flow to the heart muscle. Patients experience a feeling of tightness in the chest or left-sided chest pain (angina pectoris). If a blood clot blocks an already narrowed coronary artery, a heart attack occurs.
If the blood flow in the carotid artery and its branches is disturbed or if the carotid artery is blocked by a blood clot, a stroke is imminent. This leads to functional disorders of the nervous system such as paralysis or speech disorders.
Arteries in the pelvis and legs can also be constricted by arteriosclerosis. The so-called peripheral arterial occlusive disease (pAVK) is caused by circulatory disorders in the thighs and calves. Already after short walking distances leg pain occurs. Because those affected have to take frequent breaks from walking, it is also known as “shop window disease” (Claudicatio intermittens). Due to arterial narrowing in the pelvis, impotence can also occur in men.
Arteriosclerosis in the renal vessels leads to symptoms of impaired renal function and high blood pressure. In the worst case, kidney failure occurs.
Arteriosclerosis: causes and risk factors
It is not yet known exactly how arteriosclerosis develops. The direct cause is damage to the inner layer of the vessel wall. Among other things, this promotes the accumulation of fats. What causes this damage to the arteries – experts disagree on this. There are therefore different theories as to the mechanism of the development of arteriosclerosis.
Lipoprotein-induced-atherosclerosis hypothesis for the development of arteriosclerosis
There are two forms of cholesterol: “good cholesterol”, or HDL, which removes fat from the body and carries it to the liver, where it is broken down, and “bad cholesterol”, LDL. The latter transports fat from the liver to the body cells. The fat can then be deposited in the inner walls of the arteries and cause inflammation there. This then triggers plaque formation: White blood cells migrate into the vessel wall and take up as much LDL as possible. In the process, the immune cells swell to form so-called foam cells, causing further defence cells to appear which release pro-inflammatory substances. Together with blood cells and foam cells, they form a growing “fat strip” in the arterial wall – the basis for arteriosclerotic plaques.
Response-to-injury hypothesis for the development of arteriosclerosis
According to this hypothesis, the trigger for arteriosclerosis is a mechanical injury to the inner arterial wall layer. It can be caused by high blood pressure, for example. The body reacts to the injury with growths and the formation of foam cells – hearth-shaped plaques develop.
Infection hypothesis for the development of arteriosclerosis
According to this explanatory model, the inner vessel wall is damaged by toxins from certain bacteria, viruses or immune reactions.
Arteriosclerosis risk factors
Older people suffer more frequently from arteriosclerosis. It also affects more men than women. Experts see the reason in female hormones, mainly oestrogen, which is said to have a protective influence. Men also develop arteriosclerosis earlier than their female counterparts.
In addition, the genetic make-up plays a role (genetic predisposition). If close relatives (men under 55, women under 65) suffer from cardiovascular disease caused by arteriosclerosis, the risk for the person concerned is also increased. Hereditary lipid metabolism disorders, but also geographical origin, also influence the risk of arteriosclerosis.
Age, sex and genetic material cannot be changed by yourself. However, diet, lack of exercise, smoking, metabolic diseases such as diabetes and other aspects also promote the development of disease in all age groups. The most important risk factors are:
- Fat and calorie-rich foods lead to high LDL cholesterol levels and obesity – both factors increase the risk of arteriosclerosis.
- Lack of exercise can cause blood pressure to rise and worsen cholesterol metabolism.
- High LDL cholesterol levels promote plaque formation.
- High levels of triglycerides in the blood
- Increased blood pressure directly damages the inner walls of the blood vessels.
- Among other things, substances from tobacco smoke promote the formation of so-called unstable plaques. These are deposits in the arteries that can break open.
- Psychosocial problems: these include not only factors such as poor education, low income or unemployment, but also loneliness and mental illness such as depression or severe anxiety disorders
- Diabetes mellitus (diabetes mellitus) damages the blood vessels (angiopathy), especially if blood sugar levels are permanently or often elevated
- Rheumatoid arthritis (“joint rheumatism”) and other chronic inflammatory or autoimmune diseases
- Sleep apnoea (obstructive sleep apnoea syndrome)
- Menopause (due to oestrogen deficiency) in women
Arteriosclerosis: examinations and diagnosis
During a medical examination, the doctor will ask you about your lifestyle. In this way he can draw up an individual risk profile. He is interested, for example, in whether you smoke, get regular and sufficient exercise, how you eat or whether you have any previous illnesses that promote arteriosclerosis. He also asks about cardiovascular diseases in family members (family history).
A blood test enables the doctor to determine whether elevated blood lipids (cholesterol, triglycerides) and blood sugar levels are present. In addition, if atherosclerosis is suspected, the doctor will determine your blood pressure, weight and possibly your abdominal girth. Furthermore, he will feel your pulse, which is weaker in relevant constrictions.
The doctor pays attention to signs of secondary diseases of arteriosclerosis and carries out appropriate tests. These are, for example:
- Through so-called auscultation, i.e. listening with a stethoscope, abnormal flow sounds can sometimes already be heard above the heart, the aorta or the arteries in the neck.
- Vascular constrictions or even dilatations of arteries can be detected from the outside with a special ultrasound examination (Doppler sonography). From the results for carotid arteries, the risk of a stroke can also be estimated.
- If coronary heart disease (CHD) is present, the doctor not only performs a normal ECG, but also a stress ECG. Deposits in the inner walls of the coronary vessels can be detected by the doctor during a cardiac catheter examination. Sometimes he also inserts a small ultrasound probe directly into the coronary vessel to be examined.
- If the doctor suspects peripheral arterial occlusive disease (pAVK), he measures the walking distance that the patient can walk without a break.
- If arteriosclerosis of the renal vessels is suspected, the examiner checks the kidney function with blood and urine tests.
- Arteriosclerosis is also the most common cause of impotence. Appropriate information from the patient and an ultrasound examination can provide information as to whether there is a narrowing of the blood vessels of the penis (or in the pelvis).
The extent of the vasoconstriction can also be revealed using other imaging techniques. X-ray examinations (including CT) or magnetic resonance imaging (MRI) with a contrast medium can be used to visualise the blood vessels.
Arteriosclerosis: Treatment
In principle, arteriosclerosis can be treated with medication or surgery. Which therapy is used in each individual case depends on the extent of the vascular constriction and the impending complications. However, it is even more important to eliminate risk factors as far as possible.
Lifestyle changes and drug treatment
People who already have arteriosclerosis or an increased risk of the disease can slow its development or progression by changing their lifestyle. In the early stages, the plaques in the blood vessels can even recede. Make sure you eat a healthy diet and get enough exercise. For some patients, a cholesterol-lowering diet may be useful. Overweight should be reduced, stop smoking and avoid permanent negative stress.
Specific diseases that increase the risk of arteriosclerosis must be treated. These include, for example, diabetes mellitus or chronic kidney failure.
Antihypertensive drugs (ACE inhibitors) can also reduce the risk of arteriosclerosis. Other active ingredients reduce the unfavourable blood fat values, such as statins, fibrates or substances that inhibit the absorption of cholesterol in the intestine.
For the drug treatment of advanced arteriosclerosis, the same drugs are often used as for the treatment of some cardiovascular diseases. These contain active ingredients that can inhibit blood coagulation and thus prevent the formation of a blood clot (thrombus). Examples are acetylsalicylic acid or clopidogrel.
Surgical treatment
Life-threatening effects of arteriosclerosis, such as advanced coronary artery disease or the threat of occlusion of the leg arteries, must be treated surgically (or interventionally). The choice of treatment depends on the type and extent of calcification.
- Balloon dilatation with vascular support: A small balloon catheter is pushed through the bloodstream to the narrowed area and inflated. This dilates the vessel and allows the blood to flow freely again. If there is a threat of renewed vascular occlusion or if the arteriosclerosis is very pronounced, a small wire mesh (stent) is inserted into the vessel at the same time to keep it open.
- Bypass: The surgeon creates a “bypass” which guides the blood past the narrowed area. To do this, he uses either the body’s own vessel (usually a piece of vein from the lower leg or a mammary artery) or a plastic vascular prosthesis.
- Operation of a narrowed carotid artery (carotid stenosis): In the case of a narrowed carotid artery, a surgical operation is usually also performed. The narrowing is often scraped out of the artery. To do this, the doctor makes an incision in the affected area, exposes the artery and removes the atherosclerotic deposits.
Arteriosclerosis: course of disease and prognosis
The course and prognosis of atherosclerosis depends on various factors:
- Location of critical plaques and vascular changes
- The extent of the vascular constrictions (stenoses) and the length of the stenoses that impede the blood flow
- Patient’s state of health: People who have had a heart attack or stroke are at greater risk
- Elimination of risk factors (lifestyle changes, treatment of triggering metabolic diseases)
The earlier you decide to change your lifestyle, the better the prospects. This is because arteriosclerosis can lead to severe secondary diseases – such as coronary heart disease.