Erysipelas: causes, signs, complications
Erysipelas: causes, signs, complications
Erysipelas is a localized inflammatory disease of the skin. It often occurs on the lower legs, but can occur anywhere on the body. In most cases bacteria use small injuries of the skin to penetrate into deeper skin layers. If erysipelas is detected early and treated effectively, erysipelas is easily controlled. Here you can learn more about the erysipelas.
Erysipelas: Description
Erysipelas, also known as erysipelas, is a skin disease caused by bacteria. Through small wounds on the surface of the body, bacteria can get into deeper skin layers and multiply there. The body tries to fight these bacteria and the skin becomes inflamed. A flat, usually sharply defined redness and painful swelling develops. Since the inflammation spreads around the point of entry of the pathogen, the appearance is reminiscent of a rose blossom, hence the name erysipelas.
Diseases such as erysipelas can also cause blisters and pustules to form in the affected skin areas and swell nearby lymph nodes, such as in the knee or groin. The affected people feel ill and develop a fever, but often do not notice the erysipelas until a few days later due to the pain and swelling.
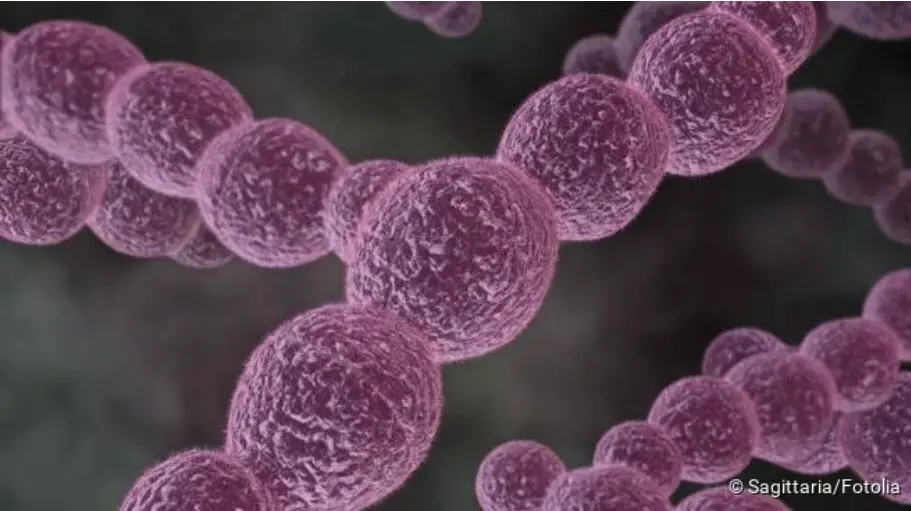
In general, bacteria can attack any area of the skin. Frequently, erysipelas occurs on the leg or sometimes also on the face. The bacteria are usually streptococci (A,C,G), more rarely staphylococci, both of which respond well to antibiotics. Erysipelas can be treated quickly, but it must be detected correctly and early on, because the infection can spread further in the body and lead to blood poisoning (sepsis), heart inflammation (endocarditis), or kidney inflammation (glomerulonephritis). It is also important to distinguish erysipelas from other diseases, as it can also be confused with thrombosis, other inflammatory processes or even a tumour.
Even after successful treatment, erysipelas can reappear within a few months (recurrence). This is unfortunately very typical, because people with skin injuries or skin diseases are always new targets for bacteria. The pathogens have it particularly easy when the immune system is weakened. This is why older people in particular are also affected by erysipelas.
Many people fear that erysipelas is contagious. However, the erysipelas does not spread from one person to another. Many other diseases caused by the same bacterium (mainly Streptococcus pyogenes) are highly contagious. For example scarlet fever, or a skin disease called contagious impetigo. However, in these cases the pathways of infection and the spread of the pathogen are different. In 20 percent of all people, Streptococcus pyogenes is already living on the skin and mucous membranes without making those affected ill. Only when it breaks through the skin barrier can disease occur.
Erysipelas: symptoms
The main symptom of erysipelas is the typical, usually sharply defined painful swelling of the skin. However, it often happens that the redness of the skin is not the first symptom or causes most of the complaints. Sometimes patients even go to the doctor for unspecific complaints without having discovered the skin change. Already at the beginning of the infection fever, headache and a strong feeling of illness can occur. The redness may not be visible at this time, but often the skin is already burning or hurting. Shortly afterwards, the swollen, red erysipelas forms around the entry point of the bacteria. Typical signs of the skin area affected by erysipelas are
- Heating
- Swelling (edema)
- Pressure pain
- flat redness
- Swelling of the nearby lymph nodes
Erysipelas: causes and risk factors
Erysipelas is an inflammation of various layers of skin caused by bacteria, which spreads to all sides and thus causes the reddish inflammatory courtyard to form. The erysipelas is mainly caused by a certain type of streptococcus: Streptococcus pyogenes. But other streptococci, or in some cases staphylococci (another genus of bacteria), can also cause erysipelas. However, they are much rarer.
Streptococci occur naturally on the skin and mucous membranes of most people without causing any symptoms. The skin acts as a natural barrier that protects us from diseases and infections. The surface of the body is colonized by bacteria that do not make us ill because they cannot penetrate the body. On the contrary, they often prevent even more dangerous bacteria from attacking the skin. However, if skin injury occurs, these bacteria can penetrate into deeper layers of the tissue and cause inflammation.
It is important to understand that mere contact with the bacterium does not make you ill, but there must always be a skin lesion. This injury can be a scratch, graze, or cut, but also dry, cracked skin, or athlete’s foot. As soon as the protective function of the skin is impaired, bacteria can penetrate the body surface.
Factors favouring erysipelas
Diseases that are harmful to the skin can promote erysipelas. A typical example is lymphedema after breast surgery. In the case of breast cancer, in addition to the tumour, important lymph vessels are also severed or removed, which normally drain the tissue. This fluid now remains in the tissue and the skin swells. This makes it easier for bacteria to penetrate the skin and cause inflammation. Swelling (edema) therefore favours the development of an erysipelas. Causes for swelling or fluid in the tissue can be:
- Heart failure
- Kidney damage
- Varicose veins
- Lymphedema
- Malnutrition
- Circulatory disorders
Diseases of the skin that impair the protective function are also risk factors for erysipelas:
- Skin fungus
- dry, cracked skin
- Neurodermatitis
- small injuries of the skin or the nail bed
Even if bacteria can penetrate the top layer of skin, the immune system often manages to eliminate these bacteria quickly and allow the skin injury to heal. A functional immune system and an undisturbed blood supply to the skin and underlying tissue is therefore very important. Some diseases or therapies disrupt the blood supply or suppress the immune system, so that in these cases bacteria can spread undisturbed in the tissue. These include, for example:
- Diabetes mellitus
- Chemotherapy for cancer
- Arteriosclerosis
- Alcohol addiction
- HIV/AIDS
Especially children and elderly people are more often affected by red blood cells. On the one hand because of their less efficient immune system, on the other hand because they injure themselves more quickly and thus there is no longer a skin barrier.
Erysipelas: examinations and diagnosis
The erysipelas is a diagnosis that the doctor already makes on the appearance and symptoms. Depending on the stage of the disease, general indications of infection can also be found. A rise in temperature (fever), changes in the rate of blood sedimentation and other changes in blood values help the doctor to assess the physical response and the severity of the infection. Unfortunately, wound swabs for pathogen detection are rarely helpful in erysipelas and bacterial cultures can only be obtained from the blood when large numbers of bacteria have already entered the bloodstream.
It is particularly important to look for the entry point of the bacteria. For example, pimples or small tears in the skin at the corners of the mouth (rhagades) are often responsible for erythema on the face.
In addition, the doctor must clarify which risk factors or diseases favour the development of erysipelas.
The difficulty in diagnosing erysipelas is to exclude other causes. A variety of diseases can cause redness and swelling of the skin and each one requires a specific therapy. Therefore it is important to distinguish exactly which disease the patient has. In this situation, the doctor must also consider, among other things, a thrombosis with subsequent tissue inflammation (congestive dermatitis), borreliosis after a tick bite, or an allergic reaction.
Erysipelas: treatment
You can read how erysipelas is treated in the article Erysipelas – Therapy.
Erysipelas: course of disease and prognosis
If erysipelas is detected early and treated correctly, the prognosis is generally good. Common entry points are injuries to the nail bed or athlete’s foot. People with a weakened immune system and disturbed blood circulation are particularly affected. In order to prevent the recurrence of erysipelas, regular medical foot care is recommended for people with an increased risk such as diabetics. Often the doctor is only consulted when fever and physical discomfort occur and an adequate therapy is started.
Possible complications of erysipelas.
If treatment is not carried out or is not successful, serious consequences may result. For this reason it is important to stop the course of the disease as quickly as possible.
In the case of lymphedema, the skin barrier is often disrupted, so that erysipelas can occur. If erysipelas occurs more frequently, the lymph vessels are damaged by the inflammatory processes. As a result, there is a permanent, often massive swelling of the affected area (elephantiasis nostras). This swelling, in turn, promotes a renewed erysipelas.
This vicious circle can only be broken by efficient treatment. If left untreated, erythema can spread into deeper skin layers (phlegmons), causing considerable damage to body tissue and organs. In addition, the bacteria can enter the blood and cause blood poisoning (sepsis). In this way, an additional inflammation of the inner wall of the heart (endocarditis) may occur, or the filtering apparatus of the kidney may become inflamed (glomerulonephritis). Especially in the case of erysipelas in the face, inflammation of the meninges can develop without treatment (meningitis).
However, all these potentially life-threatening complications can be prevented by early and consistent treatment of the erysipelas and therefore occur very rarely in Western countries.





