Knee Bursitis
Knee Bursitis
Some joints are particularly susceptible to Inflammation of the bursa sac: Knee-Joints are also among them (Source). Bursitis is inflammation or irritation of a bursa sac (Source). You have these sacs all over your body (Source). Therefore, bursitis is a standard condition that can appear in your knee, as knee bursitis (Source). There are several bursa sacs on the knee, which can become inflamed or irritated due to incorrect or excessive strain (Source).
Accordingly, a distinction is made between bursitis prepatellaris or prepatellar (Source) and bursitis infrapatellaris, for example (Source). Some occupational groups are particularly susceptible to bursitis of the knee (Source). If the doctor finds an inflammation of the bursa in the knee, knee bursitis, it is usually the bursa in front of the kneecap or the one under the kneecap that is affected (Source).
Read more about this topic here below! If you want to read about bursitis in general, we have this article here.
ICD codes for this condition are M70 and M71

- What’s a bursa sac?
- Causes: What causes bursitis of the knee?
- Diagnosis of bursitis of the knee
- Therapy of bursitis of the knee joint
- How can I prevent knee bursitis joint?
- When is a bursa operated on?
- What is the duration of sickness in the case of bursitis of the knee?
There are several bursa sacs in the knee joint that can become painfully inflamed: above the patella (Bursa praepatellaris), in front of and behind the patellar tendon (Bursa infrapatellaris) and inside the knee joint (Bursa Pes anserinus).
Bursae are hollow spaces filled with liquid and lined with joint mucosa (synovialis). The chronic inflammation of a bursa is called bursitis. The function of the bursae is to reduce friction and pressure in the tissue where tendons, muscles, and bones move against each other.
The symptoms of knee bursitis are stabbing knee pain, pressure pain, or extension deficits of the knee joint. Often the causes are unclear. Work in the knee, impact, and trauma, but also deposited uric acid crystals (gout) are among the causes of knee bursitis joint. Often, conservative therapy of bursitis is successful with the help of anti-inflammatory drugs and physiotherapy. In the case of chronic bursitis, there is usually only one operation that helps: the inflamed and scarred bursa on the knee is then removed in a minimally invasive operation.
What is a bursa?
A bursa (bursa synovialis) serves as an elastic, fluid-filled, and freely movable cushion for all the body’s movement organs. Bursa synovialis protect muscles, tendons, and ligaments during movement and loading of the knee joint: As damping organs and sliding surfaces, they enable a smooth, inflammation-free movement sequence.
Causes: What causes bursitis of the knee?
- Trauma and impact on the bursa of the knee
- Overloading, e.g. when working on your knees (tilers, gardeners)
- Friction due to crystal deposits (uric acid crystals in gout)bacterial inflammation, e.g. after injuries
Bursitis of the knee can have various causes. Bursitis is often caused by permanent irritation and pressure. Professionals who do their work on their knees, such as tilers, are particularly affected. But also athletes, e.g. soccer players or wrestlers, can be affected by bursitis of the knee due to the permanent irritation. Other causes of bursitis can be injuries, contusions, infections, rheumatic diseases, poor immune defense, or autoimmune diseases.
Symptoms of bursitis of the knee
Initially, the patient notices a rubbing sensation during movement. In the case of more severe inflammation, more synovial fluid is formed. This results in an effusion that feels firm and elastic. In addition, many patients suffer from pressure pain, swelling, overheating, knee pain when moving, and sometimes redness.
Inflammation of the bursa in the knee leads to pain and swelling. The knee feels overheated and in some cases, redness is directly visible from the outside.
Diagnosis of knee bursitis
After a detailed anamnesis (questioning of the patient), the doctor examines the affected knee. The typical palpation usually allows the doctor to determine very quickly whether there is inflammation of the bursa. In addition, the ultrasound reveals inflammation of the bursa as a kind of fluid-filled cushion.
If it is an inflammatory reaction that has already been going on for some time, the edges of this “water sack” may already be thickened. Although inflammation of the bursa is a relatively easy diagnosis for the doctor to make, other basic diseases must nevertheless be excluded by the previous anamnesis or possibly by further examinations.
Treatment For Knee Bursitis
Normally, bursitis can be treated conservatively. It is important to protect, immobilize, and cool the affected knee. This is usually done with the help of splints. The leg must be positioned high up. Pain-relieving and anti-inflammatory drugs (e.g. ibuprofen, diclofenac) are used to support the faster healing process. Severe effusions can be punctured to reduce pressure and tension. Laser and ultrasound therapy are also used.

As a result of the inflammation, bursae can scar and lose their elasticity. Recurrent inflammation then becomes more and more likely. In many cases, only surgical removal of the bursa (bursectomy) is an effective therapy for bursitis of the knee.
Cell biological regulation therapy (matrix therapy) for bursitis
Biomechanical stimulation (BMS) with a special vibration massage effectively reduces inflammation in the soft tissue. The vibration treatment involves all muscles and tendons in the vicinity of the knee joint. Via the tendon tension, the vibration is transferred to all soft tissue and bursae and effectively supports the healing of bursitis.
In addition to providing relief and anti-inflammatory treatment, cell biological regulation therapy (ZRT®-Matrix-Therapy) improves the metabolism in the region of the inflamed bursa by the gentle mechanical oscillation of the tissue. Signs of inflammation and pressure sensitivity of the bursa usually disappear after a few treatments with the Matrix-Therapy.
Physiotherapy and exercises for knee bursitis
It is important to get the joint moving again in good time after the resting phase in order to avoid relieving postures and restricting movement. You should, therefore, consult your doctor as to how long the immobilization should take place. You should then perform specific movement exercises. The following exercises can support you in this.
Exercise: Knee pendulum
Exercise knee pendulum: The pendulum stimulates the formation of synovial fluid.

Starting position: Sit on a table or horizontal surface. The affected leg hangs freely. The feet do not touch the floor.
Technique: Let the hanging leg swing slowly back and forth without muscle tension. Your hands should grasp the thigh above the knee joint and perform rhythmic traction while swinging. This mobilizes the tissue above the knee.
Repeat 20 times per leg. This is one set. Perform 2-3 sets with about 30 seconds break between each set. Practice 2 to 3 times per week.
Exercise: Mop the floor
Practice mopping the floor: This exercise improves the mobility of the knee joint and reduces knee pain.

Starting position: Sit on a stool with a bent leg. The foot stands on a cloth lying on a floor with little resistance (e.g. parquet/tiles).
Procedure: Wipe the floor with your foot by extending and pulling the leg in the knee joint. Execute the movements evenly.
Repeat the exercise 20 times per leg. This corresponds to one set. Do 2-3 sets with about 30 seconds break between each set. Practice 2 to 3 times per week.
Exercise: Improvement of the stretching
Starting position: Supine position, with the affected leg, stretched out. If full knee extension is not yet possible, you can place a rolled-up towel under the hollow of the knee.
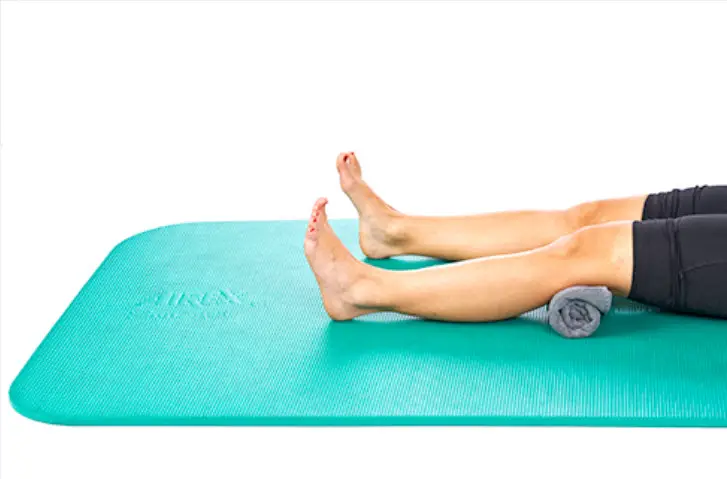
A towel in the hollow of the knee can help you to perform the exercise.
Procedure: Tighten the toes and press the knee onto the towel roll. Try to press the hollow of the knee into the ground. Hold this position for 5 to 10 seconds and then return to the starting position.
Repeat the exercise 20 times per leg. This corresponds to one set. Do 2-3 sets with about 30 seconds break between each set. Practice 2 to 3 times a week.
How can I prevent the knee bursitis joint?
Avoiding triggering factors is central to the effective prevention of knee bursitis. However, prevention is not possible for all causes. In the case of rheumatic diseases, autoimmune diseases, etc., the therapy depends on the underlying disease. If the bursitis is based on a permanent and excessive strain, it makes sense to take measures to prevent a renewed inflammation. Those affected should avoid long, monotonous movements. The same applies to constant pressure and constant strain.
Possibilities for prevention
In the case of repetitive one-sided movements, you should take breaks and acquire compensatory movements. Cushions (e.g. knee pads) protect the highly stressed parts of the knee joint in case of unavoidable stress.
Strengthened muscles help to stabilize and relieve the strain on your knee joint. Regular stretching and strengthening exercises are therefore recommended. The following exercises strengthen the knee joint and can prevent bursitis.
Exercise: Stretching of the ischiocrural musculature
Exercise Stretching the ischiocrural muscles: This exercise stretches the back of the thigh.

Starting position: Supine position on a mat. The hands grasp the thigh of the leg to be stretched and pull it towards the chest until maximum flexion of the hip joint is achieved.
Performance: Stretch the leg upwards until a distinct feeling of tension is felt in the back of the thigh.
Hold the stretch for at least one minute per leg. This corresponds to one set. Perform 2-3 sets with about 30 seconds break between sets. Practice 2 to 3 times per week.
Exercise: Stretch the quadriceps muscle
Exercise to stretch the thigh muscle (quadriceps): This muscle contributes significantly to the stabilization of the knee joint.

Starting position: prone position on a mat. Grasp the leg to be stretched by the ankle joint. If you find this difficult, a belt or towel can be used as an arm extension.
Procedure: Press the pelvis into the ground. Tense the gluteal muscles. Now pull the affected leg towards the buttocks with your hand or a towel or belt until a clear feeling of tension is felt in the front of the thigh. Avoid a hollow back.
Alternative standing with a towel: Stand on one leg with your upper body straight. You can hold on to a wall or chair back to stabilize your balance.
Procedure: Wrap the towel around the leg to be stretched at the ankle joint and pull the foot towards the buttocks until a distinct feeling of tension is felt in the front thigh. Avoid a hollow back.
Hold the stretch for at least one minute per leg. This corresponds to one set. Perform 2-3 sets with about 30 seconds break between each set. Practice 2 to 3 times a week.
Exercise: Stretching of the gastrocnemius muscle
Exercise for stretching the calf muscle (M. gastrocnemius).

Starting position: Standing in front of a wall. Place the leg to be stretched backwards.
Procedure: Support yourself with your hands lightly against the wall. Bend the front leg and at the same time push the heel of the back leg towards the floor. You should feel a distinct feeling of tension in the back of the lower leg. The leg that is to be stretched is stretched as much as possible in the knee joint.
Hold the stretch per leg for at least one minute at a time. This corresponds to one set. Perform 2-3 sets with about 30 seconds break between each set. Practice 2 to 3 times a week.
Exercise: Knee extension
Exercise with the gymnastics ball: This exercise strengthens the thigh muscles and prevents knee pain.

Starting position: Stand in front of a wall. A gymnastic ball is trapped between the wall and your back. The legs are stretched out. The feet are a little bit in front of the knees.
Performance: Roll down the wall very slowly. Rolling down the wall is the main focus of the exercise. The bending angle in the knee joint should not exceed 40 degrees. Pay attention to a straight leg axis: the knees should not fall inwards or outwards during the exercise. Then they roll up again.
Repeat the exercise 10 times per leg. This corresponds to one set. Do 2-3 sets with about 60 seconds break between each set. Practice 2 to 3 times per week.
Exercise: Squats
Exercise: Squats strengthen the leg muscles.

Starting position: Stand, feet standing shoulder-width apart.
Execution: Slowly bend your knees while keeping your arms stretched forward. The flexion angle in the knee joint should not exceed 40 degrees and the knees should not extend beyond the tips of the feet in the final position. Also, make sure that your knees do not bend inwards or outwards during the execution.
Repeat the exercise 10 times. This corresponds to one set. Perform 2-3 sets with about 60 seconds break between each set. Practice 2 to 3 times a week.
Exercise: Strengthening the calf muscles
Exercise Lower Heels: This exercise stretches and strengthens the calf muscles.

Starting position: Both feet are parallel to each other on a low step. The heels protrude over the edge and float in the air. The balls of the toes carry the body weight.
Execution: Stand on tiptoe and let yourself sink slowly until your heels are just above the ground but not touching it. As you descend, your entire body weight is slowed down by the calf muscles. Then slowly push yourself up again.
Repeat the exercise 10 times. This corresponds to one sentence. Perform 2-3 sets with about 60 seconds break between each set. Practice 2 to 3 times per week.
When is a bursa operated?
What are the advantages of an operation?
- Conservative therapy cannot successfully treat bursitis of the knee.
- Recurrent (chronic) bursitis occurs.
- This is a bacterially caused, purulent bursitis.
In case of a bacterially caused bursitis, an operation may be necessary for which both the pus and the entire bursa are removed. This procedure is called a bursectomy. In addition, bacterial bursitis is always treated with antibiotics to fight the inflammation. The aim is to prevent the bacteria from entering the bloodstream (sepsis) and thus prevent the bacteria from spreading further.
Instead of the removed bursa, a new, unscarred bursa is formed by the body within a short time.
How long is the sick leave for knee bursitis?
The duration of sick leave in the case of bursitis depends on the course of the inflammation and your profession. In many cases, the doctor will only write you off sick for a few days in the case of acute bursitis of the knee. After that, you may resume sedentary activities and office jobs. People who work hard and put excessive strain on their knee joint need a longer sick leave. Sick leave can last up to six weeks in the case of acute inflammation.
In the case of chronic bursitis, surgery is often necessary to prevent sepsis (blood poisoning). After an operation (bursectomy), sick leave lasts about two to four weeks. However, even after this time you should take care of your knee for a few weeks and wear an orthosis if necessary to relieve the pressure on the knee joint. Physiotherapeutic support can be helpful during this time.
Summary
The first case is called bursitis praepatellaris, the second case is called bursitis infrapatellaris. However, there are other bursae in the area of the knee joint that can become inflamed (like the bursa anserina).
However, the cause of pain in the knee area is not always bursitis. The hollow of the knee and the area of the thigh near the knee do not contain bursae. The same applies to the region to the side of the joint space. If pain occurs in these areas, another cause must, therefore, be sought. For example, this could be a Baker cyst – a fluid-filled cavity in the hollow of the knee.
Bursitis praepatellaris
Doctors refer to an inflammation of the bursa directly in front of the kneecap (Bursa praepatellaris) as Bursitis praepatellaris. The affected bursa is located directly under the skin and guarantees that the kneecap can move in relation to the skin on the knee.
Bursitis in this region occurs particularly in people who expose their kneecaps to high pressure. These are for example tile installers, carpet layers, and rug installers. Most of the work in these trades have to be done kneeling, which places excessive pressure on the bursa in front of the kneecap.
This is why in English, the Bursitis praepatellaris is therefore also called “carpet layer knee”. Many professional associations require the wearing of knee pads at work in order to prevent such bursitis of the knee.
Bursitis praepatellaris also often occurs after gardening work or after a fall on the knee.
Bursitis infrapatellaris
Bursitis infrapatellaris is an inflammation of the bursa below the patellar tendon (directly below the kneecap). This inflammation of the bursa is less common than bursitis praepatellaris, but is also often caused by long knees – for example when kneeling upright on a kneeler when praying. This is why Bursitis infrapatellaris also has the English name “clergyman’s knee”. The most common name anyway is “knee bursitis” and that is the name we have utilized.
Long, knee-stressing sports activities can also cause irritation of the bursa under the kneecap. Bursitis infrapatellaris can also occur in the context of another disease (gout, syphilis). However, this is only rarely the case.
Note: The inflammation of the bursa mentioned above cannot be distinguished from an inflammation of the Hoffa fat body (Hoffaitis) during the examination. This fatty body is also important for the buffering of the tendon during movement and is located directly above the bursa. Since both inflammations are treated in the same way, the exact distinction is usually not relevant for the patient.
Pes anserinus bursitis
Just below the knee on the inside of the shin bone, three tendons are attached. This attachment (Pes anserinus superficialis) is protected by a bursa (Bursa anserina) to reduce friction between the mobile tendons and the hard bone. Although the inflammation of this bursa can be caused by pure overloading, it is often related to malposition or joint inflammation of the knee (osteoarthritis). As there are several other orthopedic causes for such an inflammation, one should always seek medical clarification – especially if there is repeated inflammation in this region.
Note: Inflammation of the bursa anserina is often difficult to distinguish from inflammation of the tendon attachments (Pes anserinus tendinose). However, this is not important for the treatment
References
- Drake, D. F., Pidcoe, P. E. & Ericksen, J. (2011). Botulinum toxin type A for nonsurgical lateral release in patellofemoral pain syndrome: a case study. Military medicine, 176(6), 696-698.
- Glombitza, M., Customs, B., & Rixen, D. (2016). Salvage procedures for knee/knee infections. Trauma and occupational disease, 18(1), 78-84.
- Habib, G. S., Saliba, W. & Nashashibi, M. (2010). Local effects of intra-articular corticosteroids. Clinical rheumatology, 29(4), 347-356.
- Heintjes, E., Berger, M. Y., Bierma-Zeinstra, S. M., Bernsen, R. M., Verhaar, J. A. & Koes, B. W. (2003). Exercise therapy for patellofemoral pain syndrome. Cochrane database of systematic reviews (Online)(4).
- Johnson, J. (2003). Treat Your Own Knees: Simple Exercises to Build Strength, Flexibility, Responsiveness and Endurance. Hunter House.
- Jonasch, E. (2019). The knee joint: diagnosis and therapy of its injuries and diseases. Walter de Gruyter GmbH & Co KG.
- Klapper, R. L. & Huey, L. (2007). Heal Your Knees: How to Prevent Knee Surgery and What to Do If You Need It (Revised ed). M. Evans & Company.
- MD, N. A. & Scali, B. (2010). FrameWork for the Knee: A 6-Step Plan for Preventing Injury and Ending Pain (Framework Active for Life) (1 ed). Rodale Books.
- Marra, M. D., Crema, M. D., Chung, M., Roemer, F. W., Hunter, D. J., Zaim, S. et al. (2008). MRI features of cystic lesions around the knee. The Knee, 15(6), 423-438.
- Niethard, F. U., Pfeil, J. & Biberthaler, P. (2009). Orthopaedics and Trauma Surgery. Stuttgart: Thieme.
- O’Keeffe, S. A., Hogan, B. A., Eustace, S. J. & Kavanagh, E. C. (2009). Overuse injuries of the knee. Magnetic resonance imaging clinics of North America, 17(4).
- Ostermeier, S. & Becher, C. M. (2011). Anterior knee pain syndrome patellofemoral pain – patellar instability; with 8 tables. German doctors’ publication.
- PhD, W. R., MD, J. K. & Thomas. (2008). Essentials of Physical Medicine and Rehabilitation (Frontera, Essentials of Physical Medicine and Rehabilitation) (2 ed). Saunders.
- Reid, C. R., Bush, P. M., Cummings, N. H., McMullin, D. L. & Durrani, S. K. (2010). A review of occupational knee disorders. Journal of occupational rehabilitation, 20(4), 489-501.
- Tschopp, M., & Brunner, F. (2017). Diseases and overload damage to the lower extremity in long-distance runners. Journal of Rheumatology, 76(5), 443-450.
- Unknown. (2007). Practice of conservative orthopedics. Thieme Georg Publishing House.
- Wittich, C. M., Ficalora, R. D., Mason, T. G. & Beckman, T. J. (2009). Musculoskeletal injection. Mayo Clinic proceedings. Mayo Clinic, 84(9).
- Wülker, N. (2005). Pocket Textbook Orthopaedics and Trauma Surgery. Stuttgart: Thieme.





