Myoma: causes, signs, risks, treatment
Myoma: Description
A myoma is generally a tumor that develops from muscle cells. Depending on what type of muscle cells is affected, a distinction is made between
- Leiomyoma: develops from smooth muscle cells. These are found on the internal organs, for example in the uterus (uterine myoma), in the kidneys and in the stomach.
- Rhabdomyoma: develops from striated muscles located at the heart and skeletal muscles.
- Fibroleiomyoma: also develops from smooth muscle cells, but also contains additional connective tissue.
The myoma belongs to the benign tumours. Benign means that the tumours grow only slowly. They do not penetrate the surrounding tissue – they do not infiltrate, they only displace it. In addition, benign tumours do not form metastases (daughter tumours).
In contrast to malignant tumours, myomas are therefore not dangerous. Nevertheless, they can also have a strong influence on the quality of life of those affected and cause dangerous complications.
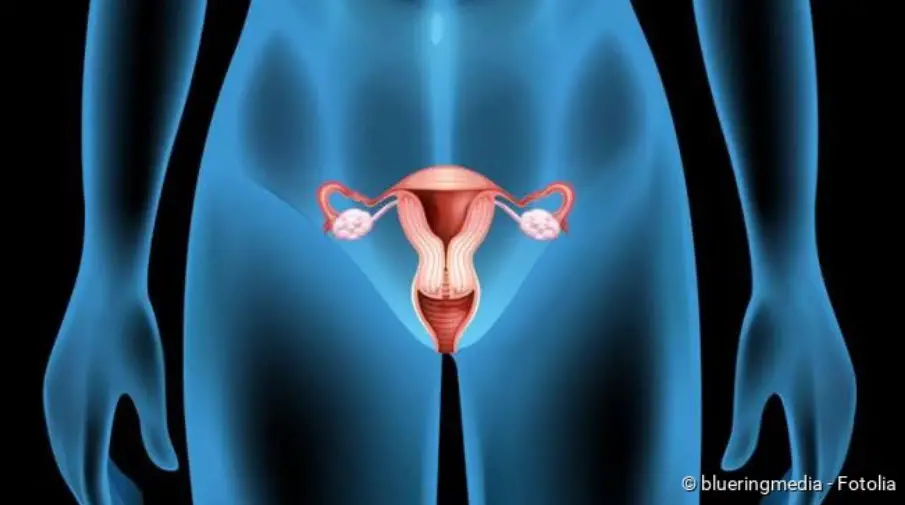
Myomas: Classification according to location
Depending on where a myoma originates in the uterus and in which direction it extends, physicians distinguish between different types of myoma:
- Subserous myoma: It is located on the outside of the uterus and grows from the muscle layer of the uterine wall outwards into the “outer” layer (serosa or peritoneum). Disorders of the menstrual period do not occur here. Sometimes subserous fibroids are stalked. This style can become twisted, which can cause pain and complications.
- Intramural myoma: Here, the myoma grows only within the muscle layer of the uterus. This type of myoma is the most common.
- Transmural myoma: Here the myoma develops from all layers of the uterus.
- Submucous myoma: This rather rare and often small type of myoma grows from the muscle layer of the uterus into the endometrium. This usually results in bleeding disorders.
- Intraligamentary myoma: This type of myoma develops next to the uterus.
- Cervical myoma: This relatively rare type of myoma develops in the muscle layer of the cervix.
What is a uterus myomatosus?
Myomas in the uterus can occur individually or in large numbers. If there is only a single tumour, experts speak of a solitary myoma. If several fibroids form simultaneously, a so-called uterus myomatosus is present. A uterus myomatosus is usually greatly enlarged and can lead to severe complications.
Facts and numbers
A leiomyoma of the uterus (uterine myoma) is not uncommon. It is the most common benign tumor in the female genital tract. About ten to twenty percent of all women over the age of 30 have a myoma of the uterus. In most cases, fibroids develop between the ages of 35 and 50. They are very rare before the age of 25.
About 25 percent of all affected women have no symptoms from the myoma. The rest had more or less severe symptoms. In 2011, about 75,600 women with a myoma in the uterus were treated as inpatients.
Myoma: Symptoms
Myomas cause no symptoms in about 25 percent of affected women. The benign tumour in the uterus is usually only discovered by chance during a routine examination by a gynaecologist.
In all other cases, fibroids cause complaints. Which these are and how pronounced they are depends on the size and location of the myoma.
Common signs of myoma are:
- Bleeding disorders: Myomas can cause increased menstrual bleeding (hypermenorrhoea), increased and prolonged menstrual bleeding (menorrhagia) and bleeding between periods outside the menstrual cycle (metrorrhagia).
- Violent, sometimes painful, pain during menstruation. In the case of heavy bleeding caused by myoma, blood clots can form, the excretion of which is accompanied by cramps.
Less common symptoms of a myoma are:
- Lower abdominal pain
- Back pain and/or leg pain when the myoma presses on areas of the spinal cord where nerves emerge.
- Kidney or side pain
- Strong urge to urinate when the myoma presses on the adjacent bladder.
- Constipation (constipation) when the myoma presses on the adjacent rectum.
- Libido pain
You can read more about dysfunctions of neighbouring organs (such as the intestine) and other complications of myoma (e.g. in case of pregnancy) in the section “Course of disease and prognosis”.
Myoma: causes and risk factors
How exactly a myoma in the uterus occurs is still unknown. Scientists suspect that the female hormone estrogen plays an important role in this process. Oestrogen ensures the growth of the mucous membrane that lines the uterus inside (endometrium). It can also affect the growth of the muscle layer in the uterine wall. For example, a malregulation could be responsible for the leiomyoma of the uterus. When estrogen production decreases after the menopause (climacteric), fibroids usually no longer occur. Existing fibroids stop growing and usually even regress.
A genetic cause of myoma development is also being discussed. Myomas are more common in certain families. In addition, studies show that African women have about nine times the risk of developing myoma than European women. A single gene is thought to be responsible for the development of myoma.
Myoma: examinations and diagnosis
Complaints such as increased menstruation or an increased urge to urinate can indicate uterine fibroids. In order to investigate such a suspicion, the gynaecologist first inquires in detail about existing complaints and possible previous illnesses (anamnesis).
After the medical history has been taken, a gynaecological palpation follows (once through the vagina and once simultaneously through the rectum and over the abdominal wall). The doctor can palpate a larger fibroid as well as the presence of several fibroids (uterus myomatosus).
As a rule, the suspicion of myoma can be confirmed by ultrasound examination (sonography). In addition, the exact position and size of the myoma or myomas can be determined. The ultrasound examination can be performed through the abdominal wall or through the vagina (vaginal sonography). Mostly the variant is chosen via the vagina.
If the ultrasound does not provide an exact diagnosis (for example, in the case of a myoma in the endometrium or in the muscle wall), the doctor can perform a mirror image of the uterus (hysteroscopy) or the abdominal cavity (laparoscopy).
If the myoma presses on the ureter, it may be necessary to examine the kidneys and the urinary tract by means of ultrasound and an X-ray with contrast medium (pyelogram).
If the examination results are unclear, the doctor will sometimes order a magnetic resonance imaging (MRI). In addition, a blood test (if anaemia is suspected) and a measurement of hormone levels are carried out if necessary.
Myoma: treatment
As long as fibroids do not cause symptoms, they usually do not need to be treated. However, a check-up should be carried out by the gynaecologist every six to 12 months. Myoma, uterus and possible complaints are then assessed in detail.
As soon as symptoms or complications occur due to one or more fibroids, various treatment options are available. Decisive factors in the choice of therapy include the age of the woman, family planning (desire for children?), type and extent of the symptoms, and the location and size of the myoma. In principle, fibroids can be treated medically (GnRH antagonists), surgically (myomectomy) or by means of newer procedures (embolization, focused ultrasound). In extreme cases, the uterus can also be removed completely.
Myoma: Drug treatment
There are various options for treating myoma with medication. Progestins, control hormones (GNRH analogs), which reduce the body’s own estrogen production, or an active substance (ulipristal acetate), which changes the docking sites (receptors) for the messenger substance progesterone directly on the myoma cells, are used.
Progestins are hormones that are also contained in many birth control pills. They are an antagonist of the sex hormone estrogen. Treatment with progestins can slow down myoma growth and sometimes even shrink myomas, which reduces the symptoms or makes later surgery easier. The inhibitory effect of the progestins on the growth of the uterine lining can reduce bleeding.
GNRH analogs mimic a specific control hormone for the female hormone balance: gonadoliberin (other names: gonadotropin-releasing hormone or GNRH). It stimulates the pituitary gland to release the hormone gonadotropin in bursts, which stimulates the ovaries to produce oestrogen. However, if GNRH analogs are used continuously, the formation of estrogens is suppressed. The myoma is no longer stimulated to grow and may even shrink.
The selective progesterone receptor modulator ulipristal acetate alters the docking sites for the hormone progesterone at the myoma cells. Its activity is thereby inhibited. As a result, the myoma cells lack an important growth stimulus, the myomas shrink and myoma-related bleeding decreases. Ulipristal acetate can be used on the one hand before surgery to improve myoma symptoms and to reduce myoma size (simplification of surgery). With a so-called long-term interval therapy (active substance intake over a period of twelve weeks with breaks), myoma size and symptoms can even be reduced so significantly in many cases that surgery is no longer necessary.
Caution: The drug containing the active ingredient ulipristal acetate for the treatment of myomas is suspected of causing severe liver damage.The suspected link is currently being investigated in more detail by the European Medicines Agency (EMA). Until a final result is obtained, the following precautionary measures are recommended (status: February 2020):
- Women taking the preparation should have their liver function checked by a doctor at least once a month. To do this, the doctor measures the liver values in the blood. If they are conspicuous, the myoma medication should be discontinued and liver function should continue to be monitored for a while.
- If there are signs of liver damage, women should consult their doctor immediately. Such warning symptoms include upper abdominal pain, nausea, vomiting, lack of appetite, fatigue and yellowing of the skin or eyes.
- Long-term interval therapy: Women who have just finished a cycle of taking ulipristal acetate should not start a new interval.
- For the time being, doctors should not prescribe the drug to new patients.
Note: The active ingredient ulipristal acetate is also contained in the “morning after pill”. However, this is only taken once. In addition, there are no reports so far that it can also cause liver damage. The EMA warning therefore only applies to the ulipristal preparation for myoma treatment.
Myoma: surgical treatment
In the case of a very large myoma, severe symptoms caused by the benign tumour or multiple myomas (uterus myomatosus), surgery is the treatment of choice. Even if it is not clear whether it is a malignant tumour (sarcoma), surgery is still necessary. In most cases, the entire uterus is removed (hysterectomy), either through the vagina, rectum or abdominal incision.
If the myoma is small and the woman still wishes to have children, it is also possible to remove myomas in isolation. This is done by removing the myomas (myoma enucleation). Depending on the type of myoma, different procedures are possible. For example, the doctor can remove the myoma through an abdominal incision or through the vagina. In addition, laparoscopic removal has increased considerably in recent years. Three small punctures are made in the abdominal wall before the doctor cuts out the myoma with a long narrow tube (the laparoscope).
Myoma: Embolization
Another method of treating fibroids in the uterus is percutaneous transcatheter embolization. In doing so, the doctor closes the blood vessels that supply the myoma with nutrients. As a result, myomas regress – ideally within six months to a maximum of one year.
Myoma: Focused ultrasound
For fibroids that are in a favourable position, another treatment option is available: focused ultrasound. The patient lies in prone position above a sound source. From there, it protects against high-frequency sound waves, which are directed at the exact spot where the myoma is located. The focusing of the sound waves generates so much heat at this point that the myoma dies off. It is then broken down by the cells of the immune system. This treatment takes about three hours and is very expensive. Since the procedure is relatively new, the costs are usually not covered by the health insurance.
Myoma: course of disease and prognosis
The course of disease in a myoma depends on the location and size of the benign tumour. Accordingly, symptoms and complications of varying severity may occur. Affected women should – even if the fibroids do not cause any symptoms – go to the gynaecologist for regular check-ups to avoid possible complications. Among the possible complications are:
- Urinary tract infections and pain when urinating when the myoma presses on the bladder/ureter
- Bladder, bowel or kidney dysfunction when the myoma presses on these organs
- Anaemia in the case of heavy and/or prolonged menstruation due to iron deficiency (iron deficiency anaemia)
- Sudden stem rotation in a pedunculated subserous myoma, causing severe pain and requiring rapid surgery
- Problems with fertility or during pregnancy
Myoma & Pregnancy
In principle, a myoma in the uterus does not represent an obstacle to pregnancy. Only in rare cases does infertility occur in affected women, for example if the myoma lies in front of the fallopian tube.
During pregnancy a myoma can cause various problems. As estrogen-dependent tumours, myomas grow faster in pregnancy because the body then produces more of the sex hormone. Due to their increasing size and location, fibroids can cause pain, positional anomalies of the child (such as breech presentation) or block the birth canal – in which case a caesarean section is necessary. Premature labour can also occur – fibroids have been shown to increase the rate of premature birth and miscarriage. If the myoma grows directly under the lining of the uterus or in the uterine cavity, this can lead to ectopic pregnancy as well as miscarriage.
No risk of cancer
Contrary to earlier assumptions, experts now no longer believe that cancer (a so-called sarcoma) can develop from a myoma. Recent genetic studies suggest that sarcoma develops independently of a myoma. Nevertheless, regular check-ups should be carried out in order to detect and treat myoma complications at an early stage.




