Neurodermatitis Of The Body And Atopic Eczema
Neurodermatitis, atopic eczema in acute attacks on the body
Neurodermatitis is a very common (8), chronic skin change that occurs on the face and/or body (1). In these cases, the skin is very dry, reddened, and itchy (7). Those affected experience a phased progression of their skin symptoms: A relapse-free (“symptom-free”) phase, in which the body skin is dry and irritated (6), but the skin symptoms can be managed (2), and an acute or “relapse phase”, in which the skin is inflamed and itches (3). During an acute episode, the application of intensive skincare (5) in combination with a medicinal treatment may be necessary (4).
What Is Neurodermatitis?
Neurodermatitis, also known as atopic eczema, is a non-contagious, chronic skin disease that affects the skin on the face and body of babies, children and adults. It is becoming increasingly common, with a two to three times increase in documented cases compared to 30 years ago. No clear cause is known, but it is now undisputed that a combination of predisposition and trigger factors can lead to the development of neurodermatitis. The altered genes lead to a disturbed skin barrier, which can no longer adequately protect against the influence of the so-called trigger factors.
Those affected have a disorder of the skin barrier and the immune system. Neurodermatitis has a phased course: In a phase free of relapse (“symptom-free”) the skin is dry, irritated and possibly slightly flaky.
In acute phases (or “push phases”) the skin becomes inflamed and itches. Even if no cure is known yet, regular intensive care can help to stabilize the skin condition and protect the skin.
In acute phases, patients typically develop skin symptoms on the face, scalp, neckline, inner side of knees and elbows, hands, wrists and feet. In babies and children, skin symptoms and affected skin areas differ.
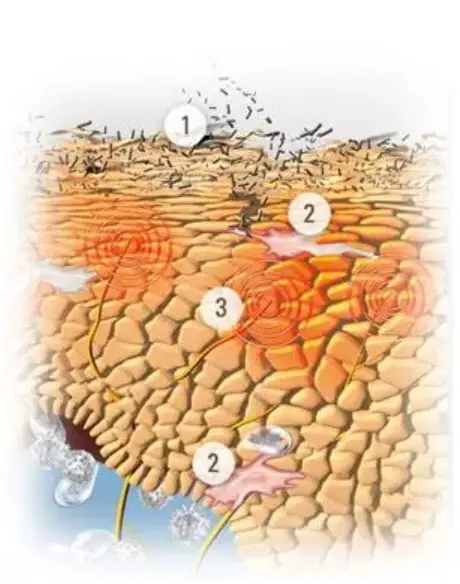
Because the skin is dry to extremely dry and itchy in acute phases, those affected scratch. Scratching additionally destroys the skin barrier. This makes the skin susceptible to infection. These bacteria cause a new irritation, which in turn causes a new itching.
Acute relapses must be treated with antipruritic, anti-inflammatory and antibacterial drugs.
Neurodermatitis can be aggravated by heat and those affected must pay attention to the tissues they are wearing. Silk or soft cotton is preferable to wool or nylon. Sweating and scratching can also lead to sleep disorders.


Consult a dermatologist if you are uncertain about your skin symptoms.
Causes And Triggers Of Neurodermatitis
The predisposition for neurodermatitis is inherited: If both parents suffer or have suffered from neurodermatitis, the child has a 60-80% risk of also developing neurodermatitis. Besides genetics, environmental factors play an important role as trigger factors for neurodermatitis. As there is no cure, avoiding these triggers and daily intensive skincare is very important, this combination can help to prolong the relapse-free phases. In acute phases, a combination of targeted skincare and medical treatment can provide rapid relief and regression of skin symptoms.
- Genetic connections. If both parents have or have had neurodermatitis, there is a 60-80% chance that the child will inherit the skin change.
- Gender. Women have a slightly higher susceptibility to neurodermatitis than men.
- Age of the mother at the birth of the child. The older the mother is, the higher the probability that the child will develop neurodermatitis.
Experts have identified various causes and influencing factors.
For example:
- There seems to be a genetic link between neurodermatitis, hay fever and asthma. If one or both parents suffer or have suffered from one or more of these diseases, this proportionally increases the likelihood that the child will develop neurodermatitis. If both parents have neurodermatitis, there is a 60-80% chance that the child will inherit the disease.
- Relationships can be established between the living environment and the risk of disease. Cities with high air pollution and cold climate increase the risk. In a study comparing Jamaican children living in London with those living in Jamaica, twice as many cases were found among London children.
- Children of older mothers are more prone to neurodermatitis than children of younger mothers.


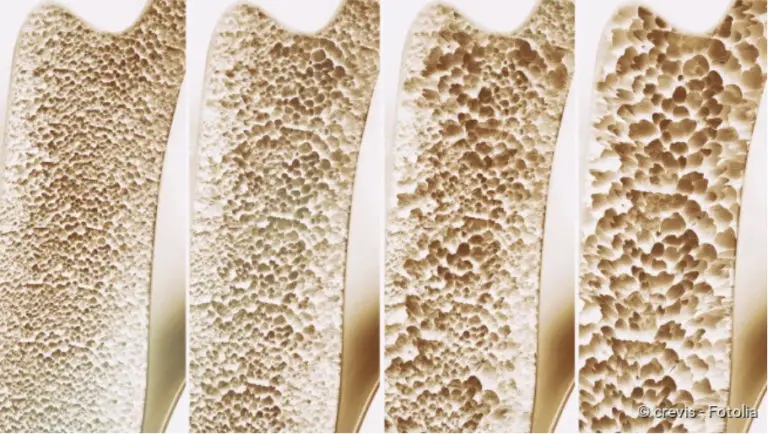
Neurodermatitis is characterized by a congenital lack of natural moisturizing factors (Natural Moisturing Factor = NMF) such as amino acids and a disruption of the metabolism of epidermal lipids.
In an acute episode, the so-called neurodermatitis cycle can be triggered, in which scratching causes a vicious circle of skin symptoms and reactions.
Neurodermatitis is inherited. Parents who suffer or have suffered from neurodermatitis, asthma, or hay fever can pass on these conditions to their child. The age of the mother can also be a factor influencing the risk of the child.
Women are generally more susceptible to neurodermatitis.
Atopic skin lacks natural moisturizing factors (NMF) such as amino acids, thus the skin barrier is disturbed. A disturbed skin barrier, in turn, makes the skin susceptible to infections and pollutants from the environment, and the skin symptoms of neurodermatitis are also its triggers. Because the skin is dry to extremely dry and itchy, those affected scratch. Scratching them destroys the skin barrier. This makes the skin more susceptible to infection. The bacteria cause a new irritation, which in turn causes a new itching. This is called the circulation of the atopic skin.
Other influencing factors
In the case of skin affected by neurodermatitis, it is important to keep it cool and reduce irritation. Among the amplifying trigger factors are:
- Clothing that makes the body sweat, for example, non-breathing nylon. You should try to avoid clothing made of non-breathing fabrics or wool – these textiles and materials can cause skin symptoms. It is advisable to wear silk or cotton clothing.
- Clothing that rubs against irritated skin, for example, wool. Among other things, silk or cotton clothing is recommended, it is soft and comfortable. For example, wearing cotton gloves at night prevents scratching during sleep.
- Certain foods. These vary from person to person, but common triggers are dairy products, nuts and shellfish. Some foods, such as nuts, can trigger neurodermatitis symptoms.
- Alcohol
- House dust mites, dust, pollen or other allergens
- Detergents and cleaning agents
- Cigarette and cigar smoke
- Pollution
- Stress and insomnia can also aggravate skin symptoms.
As a summary, we can define that there are a number of trigger factors that can aggravate the skin symptoms, these are very individual for each person affected.
These include:
- Certain foodstuffs and beverages (in particular dairy products, nuts, shellfish and alcohol)
- Textiles (especially wool and nylon)
- Allergens (house dust mites, pollen, animal hair)
- Fragrances
- Detergents and cleaning agents
- Stress, sleep disorders
- Heat, sweat, dry air
- Cigarette smoke
Keep a diary of the course of your neurodermatitis and record all the accompanying circumstances. This can help to identify individual trigger factors.
Treatment For Neurodermatitis
There is currently no known cure for atopic dermatitis, but the symptoms of the acute and relapse-free phase can be alleviated by consistent, effective skincare and appropriate medical treatment. Often, however, even the most consistent skincare cannot prevent the occurrence of an acute episode and those affected must find ways to reduce the symptoms.
So as we just said, so far, no cure for neurodermatitis is known, but there are various ways in which those affected can contribute to the care of their atopic skin and perhaps even extend the intervals between relapses.
Most important is the regular skincare with moisturizing and refatting ingredients.
Among the most important ingredients in skincare for neurodermatitis we can find:
- Omega-6 fatty acids: Evening primrose seed oil and grape seed oil: They regenerate the skin’s natural protective barrier and strengthen the skin.
- Licochalcone A (an extract from the liquorice root). It is a natural ingredient that soothes the skin and reduces redness.
Treatment with drugs
Acute episodes often require the use of topical medication in addition to daily skincare.
Glucocorticoids (like hydrocortisone) are effective and fast in relieving itching and reducing inflammation. Acute episodes often require the use of a topical medication in addition to daily skincare. Glucocorticoids are considered to be the remedy of choice, but should only be used for short periods of time. However, hydrocortisone is only recommended for short-term use.
Acute episodes often require the use of a topical medication in addition to daily skincare. Glucocorticoids (such as hydrocortisone) act effectively and quickly to relieve itching and reduce inflammation. However, glucocorticoids are only recommended for short-term use and are only available on prescription.
Treatments: Daily skincare for the body
Skin symptoms vary from person to person, but there are a number of lifestyle changes that sufferers unanimously say help them cope with their neurodermatitis.
Although the trigger factors vary from person to person, there are some lifestyle changes that have been shown to be effective in those affected:
- Keep room temperature and humidity low to avoid sweating. Keep the room temperature cool but not cold. Sweating irritates the skin and causes itching.
- When itching, it is better to tap the skin than to scratch it. Both soothe the skin, but knocking does not damage the skin barrier.
- Clothing that is soft on the skin. Silk and cotton are comfortable and can be worn in several layers in winter. Scratchy materials such as wool and non-breathing fabrics such as nylon should be avoided. Among other things, clothing made of silk or cotton is recommended; it is soft and comfortable. For example, wearing cotton gloves at night prevents scratching during sleep as we also indicate in other point of this list.
- Keep skincare products in the refrigerator, as chilled creams help to relieve itching. Store creams and ointments in the refrigerator, as cooled skincare products additionally alleviate itching.
- Keep a diary to note down triggers for relapses. Take notes of what you eat and drink and potential changes in the environment to determine if they affect skin symptoms. You will inform your results to the doctor.
- Holidays in cool to moderate climate – not too hot or too cold. Some destinations have a greater therapeutic effect than others. Examples are the North Sea, Atlantic, Dead Sea, Mediterranean and mountain regions – although extreme cold should be avoided.
- Always wash new clothing before wearing it for the first time to remove excess dye and other irritants.
- Yoga, meditation and other relaxation techniques help to reduce stress, one of the triggers for acute attacks.
- Wear cotton gloves at night to prevent scratching in your sleep.
- Keep fingernails of affected children short and smooth to minimize injuries from scratching.
- Moist compresses can help relieve itching and satisfy the urge to scratch (ask your dermatologist for more information).
- Shower rather than bathing, but never with very hot water (< 32°) and not too often or too long. Showering too often can dry out the skin.
- Do not bathe for more than 5-10 minutes.
Please consult a dermatologist if you are uncertain about your skin symptoms.