Pneumonia: Causes, Signs, Diagnosis, Treatment,
Pneumonia: Causes, signs, therapy
Pneumonia occurs particularly frequently during the cold season (Source), often as a result of delayed flu infections (Source). The most important symptoms are a general feeling of illness, cough, fever, and shortness of breath (Source). In older, chronically ill or immunocompromised persons, pneumonia can be life-threatening, especially when it is related to other conditions (Source). Read all about the symptoms, risk of infection, and treatment of pneumonia here! (Source)
Pneumonia: short overview
- Typical symptoms: strong feeling of illness, fever, chills, dry or productive cough
- Causes: Infection with bacteria, viruses, fungi or parasites, inhalation of toxic fumes, smoke, aspiration of stomach contents or blood
- Particularly at risk: children, the elderly, people with heart or lung diseases, immune deficiency, diabetes, alcohol abuse
- Risk of confusion: (chronic) bronchitis, tumors, foreign bodies in the bronchi, pneumonia/ pleurisy
- Important research: Listening (auscultation) and tapping (percussion) of the lungs, X-ray, CT, ultrasound
- Treatment: consistent protection, antibiotics (for bacteria) or antifungals, treatment of symptoms (pain and fever remedies), cough suppressants, secretion-liquefying drugs
- Dangers: Oxygen deficiency (life-threatening), carry-over with a chronic course, a spread of the pathogens to other organs (meningitis, heart inflammation, etc.), blood poisoning (sepsis)
- Rare form: Pneumocystis carinii (fungal infection with a severely weakened immune system)
Symptoms
A sudden onset of the disease is typical for pneumonia. Signs such as a general feeling of illness and weakness are among the first complaints.
Further symptoms of pneumonia follow:
- Fever
- Cough with sputum (productive cough) or dry cough
- Chills
- Shortness of breath (in case of severe pneumonia)
In the case of pneumonia, the gas exchange in the lungs is disturbed. This leads to a lack of oxygen (hypoxemia) and an increase in carbon dioxide (hypercapnia). To compensate for this, people with severe pneumonia often breathe very quickly and shallower (tachypnea).
The effort of breathing causes the nostrils to swell with every breath – a clear indication of shortness of breath and thus of pneumonia. If the lack of oxygen cannot be compensated for by this, lips and fingertips turn blueish. Doctors speak of cyanosis.
In the early stages of pneumonia, the cough is initially dry. This means that no sputum (mucus) can be coughed up. As a rule, however, productive coughing occurs after a short time, with greenish-yellowish mucus being coughed up.
Every cough can cause pain in the chest, which often radiates to the lower abdomen. If there are other lung diseases such as asthma or bronchitis, they are often worsened by pneumonia.
If you are older than 65 years, have difficulty breathing, a blood pressure that keeps dropping, or are basically just confused, then it is already recommended. The advantage in the hospital is that the antibiotics are administered intravenously and act more quickly.
Atypical pneumonia can be caused by certain bacteria as well as by fungi, viruses or parasites. The cough remains dry the whole time. Significantly milder, more pronounced symptoms, but often lasting for weeks, are further characteristics of atypical pneumonia. Symptoms, as they occur in typical pneumonia, are missing, which is why atypical pneumonia is often overlooked and therefore not properly cured.
Pneumonia: symptoms of viruses or parasites
If viruses or parasites are responsible for pneumonia, different symptoms than those of bacterial pneumonia may occur. Symptoms here are often initially fever and chills. Only after a few days, a dry cough appears.
More signs: Pneumonia of viral or parasitic origin is often accompanied by difficult expectoration of mucus and an irritable cough that lasts for a long time.
Pneumonia: Symptoms in elderly people
In older people, pneumonia is often much more serious than in younger people and sometimes life-threatening. Symptoms of pneumonia in older people include coughing (often with brownish sputum) and shortness of breath.
The brownish color of the sputum is caused by blood admixtures, which originate, for example, from tears in the smallest blood vessels in the throat. Blood admixtures in the sputum are also possible symptoms of Legionella pneumonia.
Respiratory distress, which often accompanies pneumonia in older people, is due to the reduced performance reserve of the lungs in old age. Sometimes the affected persons have to be temporarily ventilated even in a hospital, as with coronavirus.
If the course of the disease is severe, older people, in particular, can also enter a kind of twilight state due to a lack of oxygen and an increase in carbon dioxide, in which they appear confused or completely apathetic to their environment. Then the treatment in hospital is necessary.
Pneumonia: symptoms in children
Children and adults often develop different signs of pneumonia. Symptoms that practically only occur in children include a bloated abdomen and headaches and aching limbs. With these complaints, parents do not immediately think of pneumonia! Pneumonia in children can often be recognized by changes in behavior, especially when the little ones cannot yet speak.
The first signs of pneumonia in children can therefore be:
- high fever
- distended stomach
- erect nostrils when inhaled
- rapid breathing (tachypnea)
- Drinking Disinclination
- Reduced appetite
- particularly high heart rate
Even in children, severe coughing, accompanied by mucus or dryness depending on the cause of pneumonia, and a general feeling of discomfort are among the classic signs of pneumonia. As in adults, coughing in children is often accompanied by greenish or yellowish sputum. Coughing up may cause pain in the chest area, which sometimes radiates to the right lower abdomen.
Pneumonia: Symptoms with a weakened immune system
People with impaired immune defenses are particularly susceptible to pneumonia. Symptoms can be more pronounced and last longer. They additionally weaken the body, so that in patients with a weakened immune system the treatment of pneumonia should be carried out in a hospital.
Weakened immune defenses occur, for example, in the context of immunosuppressive therapy. This is a treatment to limit or completely suppress the function of the immune system (for example, after an organ transplant). However, the immune system can also be significantly weakened in diseases such as AIDS or diabetes mellitus.
Pneumocystis pneumonia symptoms
People with a weakened immune system can also suffer from a rare form of pneumonia, which practically never occurs at all in people with normal defenses: the so-called Pneumocystis pneumonia (Pneumocystis carinii pneumonia). It is caused by the fungus Pneumocystis jirovecii.
Pneumocystis pneumonia usually begins insidiously with coughing and slight fever. Over time, this form of pneumonia is accompanied by symptoms such as a dry cough and increasingly severe shortness of breath (dyspnoea). Fever can also occur, but is rare.
“Cold” pneumonia
The so-called cold pneumonia is characterized by the absence of fever. However, since fever is usually one of the typical symptoms of pneumonia, cold pneumonia is often not recognized as such.
Typical symptoms of cold pneumonia are as follows:
- dry cough, no expectoration of phlegm
- no, or very low fever
- a shocky breathing
- Shortness of breath
- Chest tightness
In addition, cold pneumonia causes symptoms that do not occur in other forms of pneumonia: For example, cold pneumonia can cause back pain and cold hands in children in addition to the already known symptoms.
Bronchitis or pneumonia?
Acute bronchitis is an inflammation of the inner wall of the bronchial tree through which air enters the lungs. This causes the bronchial walls to thicken, the small blood vessels around the bronchi to swell and mucus is produced. Bronchitis is therefore associated with similar symptoms to pneumonia.
How to differentiate them from the point of view of the patient? This requires an x-ray, which shows that the lungs are inflamed. But it is not serious, because both bronchitis and pneumonia are treated by the doctor with antibiotics. It is important that you go to one if you get a fever and yellow sputum – which can be the case with both pneumonia and bronchitis.
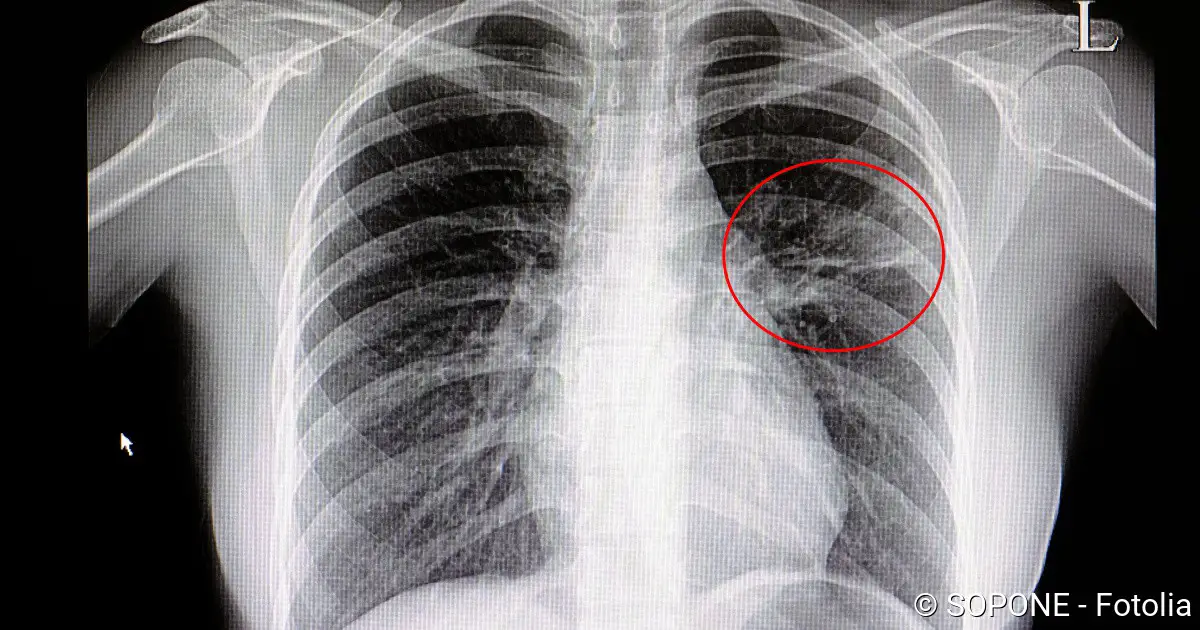
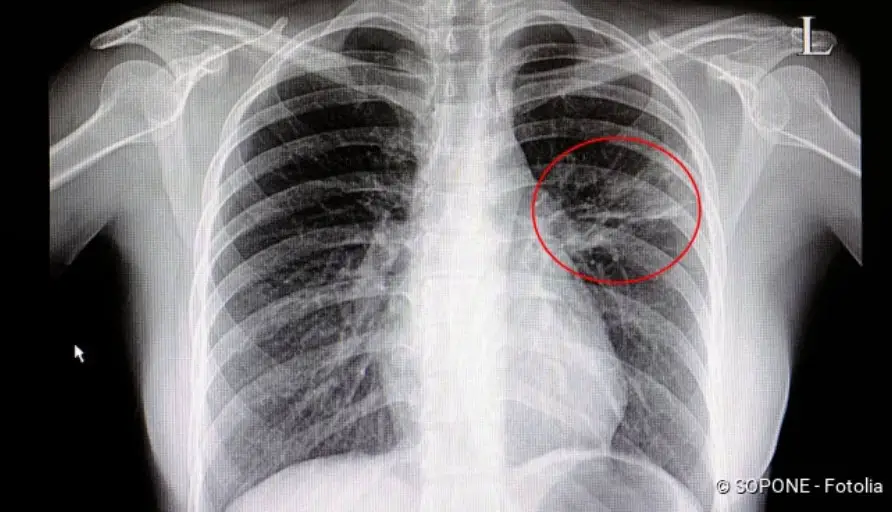
An x-ray of the chest area helps to distinguish between bronchitis and pneumonia: pneumonia is shown as shadowing in the chest area, whereas bronchitis is not visible on the x-ray. Nevertheless, the doctor often cannot give a clear answer to the question: Bronchitis or pneumonia? The symptoms of both diseases are much too similar to that.
Pneumonia: Treatment
How pneumonia is treated depends on what caused the inflammation (bacteria, viruses, fungi, parasites, etc.). The age of the patient and any accompanying or previous illnesses also play a role in the therapy.
Tip: Patients suffering from all forms of pneumonia can support their recovery by taking it easy on their bodies and drinking a lot.
Antibiotics
In bacterial pneumonia, antibiotics are almost always prescribed to kill the pathogens or prevent the bacteria from multiplying.
The earlier a bacterial pneumonia is detected and treated, the higher the probability that it will progress without complications. For this reason, antibiotics are often prescribed when the exact pathogen is not yet known. The broad-spectrum antibiotics used for this purpose are effective against many potential germs.
If the pathogen is known from a bacteriological examination of the blood or sputum, the patient can also receive a targeted antibiotic.
The duration of treatment for typical pneumonia is seven days on average but can be extended or shortened depending on the individual course of the disease. If there is no improvement after two to three days with antibiotics, the antibiotic may have to be changed or the diagnosis checked.
Anyone suffering from drug allergies, intolerance, and chronic diseases should inform their doctor before starting therapy. You should also inform him if you were abroad up to three months before the outbreak of the disease. Pathogens from other countries sometimes require a different treatment.
Antibiotic treatment is not effective for viral or any other non-bacterial form of pneumonia. Nevertheless, even then, antibiotics are often prescribed as an accompanying measure. The reason: One prevents an additional infection (superinfection) with bacteria.
Antibiotic therapy is also ineffective if individual pathogen strains have developed a so-called resistance, i.e. are insensitive to the antibiotic. Resistant bacteria are particularly common in hospitals because antibiotics are frequently used there.
As a patient, you can help to avoid such resistance formation by taking the prescribed antibiotics for exactly as long as prescribed by your doctor.
Other treatment measures
For pneumonia caused by viruses, fungi or parasites, the treatment approach is different. Depending on the pathogen, anti-fungal agents or special drugs against parasites may be necessary. In addition, drugs are used which are primarily intended to alleviate the symptoms and prevent secondary diseases:
- Antitussives (e.g. codeine, dextromethorphan) reduce the irritation of the cough in dry, irritable coughs
- Secretolytics (expectorants, for example, acetylcysteine, bromhexine) facilitate expectoration during productive coughing
- Pain and fever medicines (e.g. ASS, paracetamol) reduce the general symptoms such as aching limbs and fever
Cough blocker and cough expectorant must never be taken at the same time. Otherwise, the mucus cannot be coughed up and the shortness of breath becomes worse.
Pneumonia: outpatient treatment or hospital?
Young people without concomitant diseases can usually be treated at home. Pneumonia is then usually overcome after two, at the latest three weeks. Hospital treatment is necessary if
- the inflammation affects large parts of the lungs
- develop severe symptoms
- the patient is very old
- there is an immunodeficiency or a bad general condition
- Complications occur (for example, blood poisoning or pneumonia)
What is pneumonia?
Pneumonia is one of the most common infectious diseases. Almost one-third of those affected have to be treated in hospital. About three to five percent of those who fall ill die. This makes pneumonia the most fatal infectious disease in the European Union, to put an example, after the outbreak of coronavirus in 2020.
In pneumonia, it is mainly either the alveoli (alveolar pneumonia) or the lung tissue (interstitial pneumonia) that are damaged and can no longer function properly. This impairs the gas exchange and the body no longer receives enough oxygen. At the same time, it may release too little carbon dioxide.
The alveoli fill with aqueous or even purulent fluid. An exchange of respiratory gases in the inflamed area is only possible to a limited extent.
In some cases of pneumonia, there are many smaller centers of inflammation in the lobes of the lungs (lobular pneumonia). In others, an entire lobe of the lung is affected (lobar pneumonia, lobar pneumonia).
But not only the spread is used to characterize pneumonia. There are many other criteria of distinction:
Primary or secondary pneumonia?
If a healthy person falls ill with pneumonia without any significant health risk factors, doctors speak of primary pneumonia. If, on the other hand, there is another disease or a specific triggering event at the bottom of which pneumonia could first develop (such as asthma, COPD, cardiac insufficiency, smoke inhalation, aspiration, etc.), it is called secondary pneumonia.
Ambulatory or nosocomial pneumonia?
Outpatient pneumonia (CAP, English for community-acquired pneumonia) is caught outside a hospital. This also includes pneumonia, which someone in old people’s or nursing homes can contract. Nosocomial pneumonia (HAP) refers to pneumonia contracted in hospital (more precisely: more than two days after admission or within 14 days of discharge).
The problem with nosocomial pneumonia: In hospitals, antibiotic-resistant germs are increasingly being found, and their treatment is particularly difficult. This is because most antibiotics are no longer effective against these bacteria. The risk is particularly high for patients in intensive care units where the immune system is weakened. Artificial respiration, in particular, can promote pneumonia.
Typical or atypical pneumonia?
Pneumonia is also classified according to its course and symptoms. Doctors speak of a “typical pneumonia” when the classic symptoms of pneumonia such as productive coughing (= with sputum), fever and typical examination findings are shown in the X-ray and physical examination. Pus and water deposits clog the alveoli, which are important for the exchange of respiratory gases.
“atypical pneumonia” (also known as “interstitial pneumonia”) occurs when not the alveoli themselves but the tissue embedding the alveoli and blood vessels (interstitium) is inflamed. Atypical pneumonia is caused by pathogens other than the typical forms: mycoplasma, chlamydia, rickettsia, or legionella (all bacteria), but also fungi or parasites.
Mycoplasma pneumonia often occurs in communal facilities such as schools, homes, or barracks. Pneumonia caused by Chlamydia is caused by the genus Chlamydia pneumonia, which is transmitted exclusively from person to person. Legionella is mainly found in stagnant, warm, or hot waters. This can be lakes, showers, air conditioning or ventilation systems has a creeping, protracted course, hot water boilers, or heaters. In Legionella pneumonia, in addition to the known symptoms, confusion, lethargy and diarrhea also occur.
Special form: Pneumocystis carinii pneumonia
Pneumocystis pneumonia is a special form of this condition. It is caused by a fungus, Pneumocystis jirovecii. Healthy people are not affected by the infection. Pneumocystis carinii pneumonia mainly affects people with immune system weakness and is in most cases the first sign of infection with HIV.
Pneumonia: causes and risk factors
Infectious agents in pneumonia are usually bacteria. A certain type of bacteria, pneumococci, are responsible for half of all diseases. Infection in patients via a droplet infection is a frequent cause of pneumonia.
Many of the bacteria responsible for pneumonia also occur in the oral cavity of healthy people. However, if these germs enter the respiratory tract in large quantities, they can cause pneumonia. Sometimes the pathogens are also carried from other organs to the lungs via the blood.
Pneumonia caused by fungi usually affects people with poor general health and a weakened immune system. Parasitic pneumonia is rather rare and is also more likely to occur in immunocompromised persons or during travel to or coming from tropical countries.
Other causes of pneumonia may be:
- Bronchial congestion
- Lung tumors
- Foreign bodies in the airways
- corrosive irritants, gases, smoke or solvents
- Radiotherapy
- Inhalation (aspiration) of food, liquid, blood, stomach contents/ gastric juice
- Heart failure (cardiac insufficiency)
- Pulmonary embolism after thrombosis
- Spreading of germs via the bloodstream (hematogenous scattering) from other centers of inflammation in the body (for example in the case of bone inflammation)
Risk groups for pneumonia:
The risk of pneumonia increases especially under the following conditions:
- in elderly and weakened persons
- for chronic diseases, especially heart disease, chronic bronchitis, COPD or diabetes mellitus
- in people whose body’s own defense system is clearly weakened (e.g. in HIV infections)
- in people who are taking medication that suppresses the body’s own defenses (e.g. immunosuppressants or cytostatics)
- in alcoholic persons
- in young children
In these risk groups, it is particularly important to recognize as quickly as possible what type of pneumonia is present in order to be able to treat it appropriately. Because they are particularly at risk of infection.
Is pneumonia contagious?
Depending on its form and cause, pneumonia can be contagious. In the case of viral or bacterial pneumonia, for example, pathogens are spread in the air by coughing or sneezing and can infect other people (droplet infection).
Pediatric pneumonia
Pneumonia is the most common respiratory disease in children. It is sometimes difficult to detect, as the symptoms of pneumonia in (young) children can be very unspecific. Signs are fever, cough and high pulse, a bloated stomach, erect nostrils when inhaling, apathetic behavior, and no desire to eat or drink.
Since the immune system does not yet work as effectively in adolescents, children have little to counteract budding pneumonia. This makes it all the more important for parents to be alert and pay attention to the disease-specific symptoms. This is particularly important if pneumonia is suspected in babies and toddlers, as they cannot yet speak.
If the child has no other diseases, pneumonia usually heals within seven to ten days.
Learn more about pneumonia in children here.
Pneumonia: examinations and diagnosis
To diagnose pneumonia, the attending physician will first take the patient’s medical history (anamnesis), asking in particular about past and present illnesses and complaints, for example:
- Have you got a cough? If so, is it dry or with sputum?
- What is the nature of the sputum (quantity, consistency, color)?
- Have you noticed any chills or fever in the last few days?
- Do you have difficulty breathing or a feeling of tightness in the chest area?
- How are you feeling in general, do you feel weak and tired?
This is followed by a physical examination. The doctor tries to prove the ventilation by listening to the lungs with a stethoscope (auscultation) and the density of the lung tissue by tapping. Decreased breath sounds and compressions indicate pneumonia.
By listening to the lungs with the stethoscope, the doctor can detect reduced ventilation of the lung tissue
Blood test, urine test
A blood test also provides evidence of inflammation. In bacterial pneumonia, the number of white blood cells (leukocytes) is greatly increased. Various precursors of leukocytes can be detected in the blood. Doctors refer to this finding as a left shift. If viral pneumonia is present, the number of leukocytes is barely or not at all increased, but the proportion of lymphocytes (specialized white blood cells) is.
Legionella can be detected in urine (urine test).
X-ray examination
If pneumonia is suspected, an X-ray of the chest (chest X-ray) is always necessary. It serves to confirm the diagnosis and to identify the extent and location of the inflammation. It can also expose other diseases (e.g. tumors, lung abscesses, tuberculosis) that can trigger similar symptoms.
If no X-ray machine is initially available, suitably trained doctors can also perform an ultrasound examination to confirm the suspected diagnosis of pneumonia. If atypical pneumonia is suspected, computer tomography may also be necessary to detect even small centers of inflammation.
Bronchoscopy and bacteriological examination
Especially in atypical pneumonia, it can be important to detect the pathogen. Only then can effective pneumonia treatment often be initiated. For this purpose, a bronchoscopy is performed. The doctor inserts a flexible tube into the bronchi, which is connected to a camera and has several “working channels.
The bronchial tubes can be rinsed through these and mucus can be specifically sucked out for examination for pathogens. Other pathological changes in the bronchial tubes (constrictions, bulges, or tumors) can often be detected by bronchoscopy.
Pneumonia: Course Of Disease And Prognosis
Therapy and recovery of pneumonia proceed the better the earlier the disease is detected and treated. The prognosis also depends on the pathogen, the age of the patient, and his general (health) condition.
Several factors can have a negative influence on the course of pneumonia:
- high age
- existing heart or lung diseases
- weakened immune defense
In rare cases, complications of pneumonia may occur, which can prolong the duration of treatment. These include:
- antibiotic-resistant bacteria as causes of pneumonia
- Inflammation of the lung or pleura (pleuritis)
- Fluid accumulation between lung and pleura (pleural effusion)
- Bronchiectasis (irreversible, sack-like expansion of the bronchi)
- Formation of pus-filled cavities in the lung tissue (lung abscess)
- Inflammation of the pericardium or the lining of the heart (pericarditis and endocarditis)
- Cerebral suppuration
- Blood clot (thrombosis)
- Bone marrow inflammation (osteomyelitis)
- Joint inflammation (arthritis)
A dangerous complication of pneumonia is the spread of the pathogens via the bloodstream into other organs (haematogenic spread). For example, the meninges, heart, or ears can be affected or general blood poisoning (sepsis) can occur.
Worldwide, three to four million people die of pneumonia every year. Nevertheless, with early, adequate therapy and without existing concomitant diseases, the prognosis is good. In this case, the affected person usually recovers completely.
However, a worse prognosis can be expected if pneumonia develops during a hospital stay. Since a lot of antibiotics are used there, there is an increased risk that the bacterial strains are resistant to many antibiotic substances, which makes therapy considerably more difficult.
Pneumonia: Duration
As a rule, pneumonia therapy with antibiotics should be successful within seven days. For certain pathogens, however, longer treatment may be necessary to reduce the relapse rate (recurrence rate). After two to three weeks the symptoms of pneumonia usually subside.
However, affected people can sometimes feel worn out and listless for weeks after pneumonia and the cough can also be persistent. In order not to suffer a relapse, one should only go back to work when the physical performance is back to normal and no symptoms exist.
Sometimes, the patient affected returns to physical activity too soon or because the therapy was started with a delay.
Physicians refer to this condition that is spread over six to eight weeks as chronic pneumonia. It can cause irreversible sagging of the bronchial tubes (bronchiectasis), recurrent inflammation of the lungs, or even bleeding.
As a result, the lung tissue scars and is less elastic later. This can severely restrict lung function (restrictive pulmonary dysfunction). People with a weakened immune system or severe previous diseases of the lungs and heart are particularly at risk for delayed pneumonia.
Immunization
There is no vaccination against all possible pathogens of pneumonia. Nevertheless, a protective vaccination can often effectively prevent pneumonia. The Robert Koch Institute and other prestigious federal agencies in the US, recommend three different vaccinations, each of which is important for different groups of people and can prevent pneumonia:
Pneumococcus vaccination
A large proportion of all pneumonia is caused by pneumococci. Therefore, it is recommended that the following groups of persons undergo pneumococcal vaccination:
- all children up to 24 months
- People over 65 years of age who frequently suffer from upper respiratory tract infections
- Groups of persons with a weakened immune system
- People whose spleen has been removed
- Persons with a chronic disease (such as bronchitis, coronary heart disease, heart failure or diabetes mellitus)
Haemophilus influenzae vaccination
In about ten percent of all young patients, the bacterium Haemophilus influenzae is responsible for pneumonia. Vaccination against this pathogen is also possible.
Flu vaccination
The flu pathogen (influenza) can damage the mucous membrane and weaken the immune system. Those affected become more susceptible to pneumonia and are less able to counteract it with the body’s own defensive substances. In the following cases you should be regularly vaccinated against influenza:
- from the age of 60 up
- for cardiovascular diseases such as high blood pressure or angina pectoris
- for metabolic diseases such as diabetes mellitus
- for lung or kidney diseases
- in case of HIV infection
- for leukemia
- in daily contact with many different people
Prevent pneumonia
The best way to prevent pneumonia is a healthy, active lifestyle. A balanced, vitamin-rich diet and regular exercise improve general health and help reduce the risk of pneumonia. Tobacco and alcohol, on the other hand, should be consumed as moderately as possible – both weaken the immune system and make you an easier “victim”. Especially if you have had pneumonia before.
People suffering from a chronic respiratory disease such as asthma, COPD, or chronic bronchitis should never change or pause their basic therapy in case of an acute respiratory infection without consulting their doctor. The risk of secondary infection, possibly also with pathogens causing pneumonia, is generally increased for them.