Pulmonary embolism: symptoms, treatment, causes
Pulmonary embolism: symptoms, treatment, causes
In a pulmonary embolism (pulmonary artery embolism), a blood vessel in the lung is blocked, usually by a blood clot. The lungs are then less supplied with blood. This means that only insufficient oxygen reaches the blood. Important signs of pulmonary embolism are sudden shortness of breath and chest pain. The circulation can collapse. In the worst case, the patient dies. Here you can read everything you need to know about the symptoms, causes and treatment of pulmonary embolism.

Pulmonary embolism: short overview
- Symptoms: Shortness of breath, chest pain, anxiety, (blood) cough, dizziness or fainting
- Treatment: Stabilize breathing and circulation, administer oxygen and pain/blood thinning agents (thrombus dissolution), if necessary catheter therapy, rarely surgery
- Prevention: movement, stop smoking, compression stockings, etc.
- Risk factors: including smoking, birth control pill, heart and lung disease, advanced age, prolonged confined sitting, overweight, surgery, bedriddenness
- Examination: blood test, ECG, ultrasound, computer tomography (CT), scintigraphy
- Prognosis: high risk of death in the first two hours after onset of symptoms; improved prognosis with rapid treatment
Pulmonary embolism: Symptoms
The type and severity of the pulmonary embolism symptoms depend on the size of the diseased lung area. Very small pulmonary embolisms sometimes cause no symptoms. However, in most cases, breathing difficulties occur quite suddenly and are accompanied by chest pain. A pronounced pulmonary embolism can even lead to a circulatory collapse and in the worst case to death.
Classic symptoms of pulmonary embolism
Depending on the size of the obstructed blood vessel in the lung, the following pulmonary embolism signs occur:
- Shortness of breath and/or accelerated breathing
- Heart rhythm disturbances (racing heart, heart stumbling)
- Chest pain (may radiate to the abdomen or shoulder)
- Anxiety and restlessness
- Cough and/or haemoptysis
- Rales when breathing
- Weld outbreaks
- Dizziness or fainting spell
If very large vessels are affected by the embolism or a large area of the lung is no longer supplied with blood, the circulation collapses very quickly in the form of a shock. The blood pressure is very low. The heart still tries to pump enough blood to all organs of the body and therefore beats faster. Hands, arms, feet and legs appear cool, as they are least supplied with blood. Sometimes the lips turn bluish because they receive too little oxygen. Often the affected persons, as long as they are still conscious, are very restless and/or are very afraid.
If a large area of the lung is affected, it is also called a fulminant pulmonary embolism.
If it is detected and blood thinners are administered in time, yes. You usually get them for half a year. The problem is that the lung recovers quickly, but the clot is in the blood system. And there it can lead to the right ventricle of the heart having to withstand a higher pressure, this is called pulmonary hypertension. The heart is therefore well controlled afterwards.
If you have a congenital coagulation disorder, you can take heparin injections to keep the blood fluid before long journeys where the blood accumulates in the legs. Apart from that, the following applies to everyone: Drink a lot and stretch your legs in between so that the blood can circulate properly.
Harbingers of a pulmonary embolism
Before a blood clot blocks a pulmonary artery, small pieces of it can come loose and migrate into smaller pulmonary vessels. These small embolisms can already cause symptoms like chest pain, a whistling breath, coughing or fainting. If treatment is carried out quickly, a larger and more dangerous pulmonary embolism can often be prevented.
It is therefore essential that the complaints mentioned above be taken seriously. This is especially true in cases of shortness of breath and chest pain when leg vein thrombosis is present at the same time. Parts of the blood clot in deep leg veins can be carried along by the blood and washed into the lungs. Then we’re looking at pulmonary embolism. In leg vein thrombosis, the affected leg is often painfully swollen, reddish in colour and warmer than the other leg. If the patient was previously not mobile as usual and perhaps even bedridden, a reddened leg is already a thrombosis alarm sign. Since patients are typically inactive after surgery, the risk of pulmonary embolism is particularly high. Because without movement, the veins have a harder time keeping the blood flow going. Then blood clots form easily.
Inactivity and/or immobilization of a limb slows down blood flow. This increases the risk of a blood clot forming and causing a pulmonary embolism!
Complications of a pulmonary embolism
The larger the blood vessel that is clogged, the more severe the consequences. They can even become life-threatening for the patient. The following table lists possible consequences of pulmonary embolism and their most important symptoms.
| Complication of a pulmonary embolism | Symptoms |
| Pneumonia | breath-related chest pain |
| Entry of tissue water between the two lung leaves (pleural effusion) | Shortness of breath, breathing noises |
| Pulmonary infarction | Hemoptysis |
| Pneumonia caused by a pulmonary infarction (infarct pneumonia) | Cough, shortness of breath, fever, chills |
| Right heart failure and right heart failure | congested (thickened) neck veins, water retention in the legs |
| High blood pressure in the pulmonary circulation (pulmonary hypertension) | decreasing performance, shortness of breath under light loads, dizziness |
Some of the problems can occur quite quickly after an embolism. Others develop only after days or weeks.
Pulmonary embolism: treatment
If a pulmonary embolism is suspected, you should call the emergency doctor immediately! The patient should move as little as possible. Otherwise, further clots can become detached and block a vessel. In case of cardiac arrest, you must start resuscitation immediately!
If necessary, the emergency doctor will continue resuscitation and, if necessary, provide artificial respiration for the patient. After all, the patient’s breathing and circulation must be stabilized as quickly as possible in order to prevent organ damage (e.g. to the brain). To do this, the doctor can administer oxygen and medication to the patient, including blood thinners and painkillers. In the hospital, necessary examinations are then carried out and further measures of pulmonary embolism therapy are initiated. They depend on the severity of the disease. Patients with a severe pulmonary embolism must be monitored and treated in the intensive care unit.
Anticoagulants
In the case of a pulmonary embolism, anticoagulant drugs (called anticoagulants) are generally given. These ensure that no new blood clots form and existing clots do not enlarge. Small blood clots are broken down by the body.
Patients are often first given an anticoagulant for a few days in the form of a syringe or infusion, for example heparin. Patients then start taking an anticoagulant in tablet form.
There are now also two anticoagulants that can be given as tablets directly after diagnosis – i.e. without the need for anticoagulant injections or infusions.
The intake of an anticoagulant in tablet form (“oral anticoagulation”) must be continued for several months.
In the case of a mild pulmonary embolism, anticoagulants are often sufficient as the only therapy. If, in addition, the risk of complications is low, patients can sometimes even be treated on an outpatient (home) basis.
Drugs that dissolve the blood clot
In more severe pulmonary embolism, anticoagulant therapy is not sufficient. The blood clot in the lung must be removed in a targeted manner in order to restore the blood supply to the lung tissue. This can be achieved with certain drugs called thrombolytics (also called fibrinolytics) such as streptokinase and urokinase. They are administered directly into the patient’s blood and can rapidly dissolve the blood clot in the lungs. This form of pulmonary embolism therapy is called drug-based thrombolysis or lysis therapy.
Lysis therapy is very effective for pulmonary embolism, but can have serious side effects: In some patients it causes dangerous bleeding in the body, for example in the brain. Before this form of pulmonary embolism treatment is used, the physician will therefore weigh up the benefits and risks for the respective patient. The method is most commonly used in people with severe pulmonary embolism and unstable blood flow. These “haemodynamically unstable” patients have a high risk of (fatal) complications. That is why it is particularly important here to remove the clot in the lungs quickly.
Remove blood clot with a catheter
In some patients, drug-based thrombolysis would be too risky, for example because the risk of bleeding is too high. Then the blood clot in the pulmonary vessel can be removed with the help of a catheter instead. The catheter is carefully inserted through a vein into the affected vessel and advanced to the blood clot. Using tiny instruments, the blood clot can then be broken up into very small pieces. Some catheters also produce ultrasound waves to remove the clot. At the same time, a thrombolytic can be administered via the catheter to dissolve the clot.
The catheter is inserted through a vein and advanced to the blood clot. The clot can then be broken up using instruments on the catheter and dissolved by administering a drug (thrombolytic).
Remove a blood clot in open surgery
If pulmonary embolism treatment by catheter is unsuccessful, it may be necessary to remove the blood clot in open surgery. The procedure is called pulmonary embolectomy. The patient is given a general anaesthetic and is connected to a heart-lung machine. The latter takes over the tasks of the two organs for the duration of the operation.
As the entire operation is very risky, it is only performed in an extreme emergency.
Pulmonary embolism: causes and risk factors
A pulmonary embolism occurs when a blood-supplying vessel in the lung becomes blocked. This constipation can have various reasons.
Pulmonary embolisms due to blood clots
In most cases, pulmonary embolism is the result of a blood clot that has formed in a leg vein (leg vein thrombosis) and was washed into the lungs with the bloodstream. The reason why the clot in the leg comes loose can be quite banal, for example simply getting up in the morning, but also pressing during bowel movements and sudden physical exertion.
A pulmonary embolism occurs when part of a blood clot breaks loose and enters a pulmonary artery via the heart.
The detached clot reaches the right heart with the venous blood and is pumped from there to the lungs. As the pulmonary arteries continue to branch out and become correspondingly narrower, the clot eventually gets stuck and blocks the vessel.
Certain risk factors promote the development of leg vein thrombosis. These include:
- Smoking
- Taking the contraceptive pill or hormone replacement therapies
- Pregnancy and puerperium
- Restriction of movement (bedriddenness, plaster casts)
- Cancer diseases or treatments
- Operations (especially on the abdomen, hip or knee joint)
- Overweight
- longer flights
- Heart and lung diseases
- Blood coagulation disorders
- higher age (from 50 to 60 years)
- Thromboses in family members
- Chronic venous insufficiency, varicose veins
Other causes of pulmonary embolism
Rarely does the blockage of a pulmonary artery in pulmonary embolism have other causes than a blood clot:
Sometimes a fat embolism is behind it. In this process, fat is released from the bone marrow and migrates via the venous vessels into the lungs, where it blocks a vessel. This can happen, for example, after orthopaedic operations such as the implantation of a hip prosthesis or after a fracture of the thigh bone.
Amniotic fluid embolism is a very dangerous complication at birth for mother and child. Amniotic fluid can enter the maternal bloodstream via the wound caused by the partially detached placenta in the uterus and enter the lungs. Through various chemical processes and a form of allergic shock, thromboses form in the blood vessels. The arteries in the lungs are narrowing. The numerous blood clots trigger further embolisms. Ultimately, the heart and circulatory system can collapse.
Pulmonary embolism caused by gas (air embolism) occurs when air enters the body’s veins and is transported with the blood to the pulmonary arteries. Very rarely this can be done via vein access or by medical intervention.
Pulmonary embolism: examinations and diagnosis
Symptoms such as sudden chest pain and shortness of breath may indicate pulmonary embolism, but may also have other causes. For clarification, the doctor will first ask the patient a few questions in order to establish the patient’s medical history (anamnesis). This helps to estimate the probability of a pulmonary embolism. Possible questions from the doctor are:
- Are the lower legs swollen or reddened?
- Have you had surgery in the last four weeks?
- Have you been bedridden or have you had limited mobility for a long time?
- Do you suffer from a tumor disease?
- Have you received tumour therapy (radiation, chemotherapy etc.) in the last six weeks?
- Have you ever suffered from deep vein thrombosis or pulmonary embolism?
- Do you cough up blood?
- Is there a pregnancy?
- Are you taking the contraceptive pill or any other preparation containing female sex hormones?
The anamnesis interview is followed by a detailed physical examination to find further indications of a pulmonary embolism. For example, the doctor listens to the heart and lungs and measures the patient’s blood pressure.
Pulmonary embolism: blood tests
Certain blood values can be indicative of a pulmonary embolism diagnosis. This is because in the case of leg vein thrombosis or pulmonary embolism, the body tries to dissolve the blood clots again. This produces so-called D-dimers. These are cleavage products of the fibre protein fibrin, which is involved in the formation of a blood clot. If no D-dimers are detectable in the patient’s blood, a pulmonary embolism is very unlikely.
Other important blood values are troponin and brain natriuretic peptides (BNP). In the case of a pulmonary embolism, their blood levels are elevated.
Oxygen and carbon dioxide in the blood are also important parameters when pulmonary embolism is suspected. Since the gas exchange in the lungs is impaired in the case of a pulmonary embolism, the oxygen content in the blood drops. Breathing accelerates to compensate for this deficiency. As a result, more carbon dioxide is breathed out – its content in the blood also decreases.
Pulmonary embolism: ECG
An electrocardiographic examination can also support a pulmonary embolism diagnosis. For this purpose, several electrodes are attached to the patient’s chest, wrists and ankles and connected to a measuring device with cables. The heartbeat is recorded by a recorder. Since in a pulmonary artery embolism the heart has to pump against a higher pressure and is supplied with less oxygen, the ECG shows signs of cardiac overload.
Pulmonary embolism: ultrasound examination
An ultrasound examination of the heart (echocardiography) can show whether heart function is impaired as a result of pulmonary embolism. For this purpose a gel is applied to the chest in the area of the heart. The examiner can use the ultrasound head to view the heart cavities, valves and blood flow. In addition, the leg veins are often examined with the ultrasound machine: very often, a pulmonary embolism develops as a result of leg vein thrombosis. Ultrasound can reveal possible residual clots in the veins.
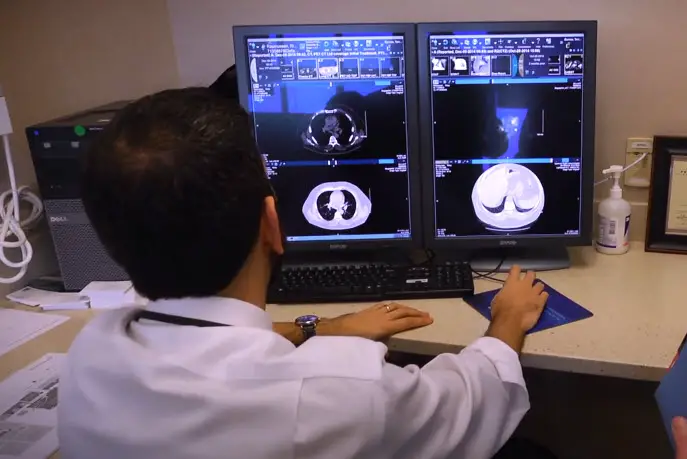
Pulmonary embolism: CT and scintigraphy
By means of computer tomography (CT) a pulmonary embolism can usually be made very clearly visible. Before the examination, the doctor injects a contrast medium into an arm vein. A CT image of the patient’s chest is then taken. The radiologist can then follow the course of the pulmonary vessels and locate thrombi.
In some cases a scintigraphy of the lungs is also performed. This is a nuclear medical examination in which the patient has to inhale a radioactively labelled substance. The images of the examination show how well the individual lung areas are supplied with blood and ventilated.
Pulmonary embolism: course of disease and prognosis
How dangerous pulmonary embolism is depends on its extent and the patient’s state of health. A pronounced pulmonary embolism is life-threatening. Acute deaths often occur within two hours after the onset of the symptoms of a pulmonary embolism. A patient’s chance of survival can be increased if a doctor is immediately notified and the correct treatment is initiated.
Once the disease has been overcome, the probability of suffering another pulmonary embolism is often increased. It is therefore important to reduce the risk of blood clots forming. This includes, for example, that patients conscientiously take the anticoagulant medication as prescribed by their doctor. This medicinal prevention can last for months or years. Some patients have to use the anticoagulants for the rest of their lives.
Further preventive measures can be found below.
Pulmonary embolism: Prevention
In general, ensure regular exercise in everyday life. This prevents the formation of blood clots and thus also a possible pulmonary embolism.
In the case of prolonged bedriddenness and diseases that promote the formation of thrombosis, the doctor often prescribes anticoagulant medication (e.g. heparin injections). They are intended to reduce the risk of thrombosis and pulmonary embolism.
Don’t smoke! This is especially true if you have already had thromboses.
After an operation you should – if possible – move again quickly. If you have to lie in bed, you can accelerate the blood flow in the veins by varying the tension of the muscles. This lowers the risk of blood clots forming.
You should also stimulate the blood flow in your legs on longer flights. If possible, get up from time to time and walk a few steps. You can also do foot gymnastics while sitting down (for example circling your feet). Drink enough, but not coffee or alcohol. Do not wear restrictive clothing. Especially if you have known vein weakness, you should wear compression stockings during the flight. Such stockings can also be useful for longer periods of bed rest and during pregnancy.
If there is a high risk of thrombosis and pulmonary embolism, a kind of sieve (cava screen) can be inserted into the inferior vena cava. It traps clots from the leg veins so that they do not enter the lungs and cause a pulmonary embolism.