Skin cancer: symptoms, cancer types, treatment
Brief overview
- What is skin cancer? Collective term for various malignant skin diseases. Every year in Germany more than 293,000 people are newly diagnosed with skin cancer. The most frequent is “white skin cancer”, followed by “black skin cancer”.
- Forms of skin cancer: White skin cancer (basal cell carcinoma and prickle cell carcinoma), black skin cancer (malignant melanoma), rare forms of skin cancer (such as Merkel cell carcinoma, Kaposi sarcoma, dermatofibrosarcoma protuberans)
- Symptoms: very different depending on the form of skin cancer and subtypes. For example, black skin cancer often appears as a dark, irregularly shaped skin patch, which can be either flat or knotty. Basal cell cancer often begins as a waxy nodule that sinks in the middle and alternately heals and bleeds again. But there are also dark, yellowish or ulcerous basaliomas.
- Causes & risk factors: In the case of white and black skin cancer, mainly UV light (sun, solarium, etc.); other risk factors depending on the type of skin cancer, for example genetic predisposition, hereditary diseases and chemicals. In rare forms of skin cancer (Kaposi’s sarcoma, etc.) among other things, viral infections.
- Treatment: depends on the type of skin cancer and the stage of the tumour. Standard method is an operation. Alternatively or in addition, other therapies can be used such as radiotherapy (radiation), chemotherapy, photodynamic therapy or immunotherapy.
- Prognosis: If skin cancer (of any kind) is detected and treated early, the chances of recovery are generally high. The more advanced a tumour is, the worse the prognosis. This is especially true for malignant melanoma.
Skin cancer: symptoms
The chances of recovery from skin cancer are better the earlier the tumour is detected and treated. But how do you recognize skin cancer? The answer depends on the exact form of skin cancer. In general, the signs of dangerous malignant melanoma (black skin cancer) are easier to recognize than those of “white skin cancer”. Malignant melanoma develops from pigment forming skin cells (melanocytes) and therefore causes dark coloured skin changes. However, the manifestations of the malignant melanoma are partly very different. In “white skin cancer” (basal cell carcinoma and prickle cell carcinoma) the skin changes are usually lighter in colour.
The following applies to all forms of skin cancer: The symptoms of skin cancer are limited to the skin in the early stages. As soon as the cancer cells spread in the body, further symptoms can develop.
In principle, all parts of the body can be affected by skin cancer. However, it most frequently occurs on skin areas that are exposed to the sun (e.g. face, ears, hands). Therefore, these regions in particular must be protected from sunlight (e.g. sunscreen, clothing, headgear, sunglasses). Always consult a dermatologist if you have newly occurring skin changes that hurt or bleed, or liver spots that change.
In principle, everyone who has been diagnosed with skin cancer has a significantly increased risk of developing further skin tumours. This is why prevention by the dermatologist is so important. In addition, a recent study has shown that patients who developed six or more basal cell carcinomas in ten years have an approximately threefold increased risk of other tumor types (e.g. colon cancer). However, this concerns only a small part of the skin cancer patients.
Black skin cancer: symptoms
Black skin cancer (malignant melanoma) can look like a simple pigment mark (mole, birthmark). On the basis of the so-called ABCD-rule it can be estimated whether a dark mole is actually a harmless pigment mole or possibly a black skin cancer. You can read more about this in the section “Skin cancer screening”.
Essentially there are the following manifestations of malignant melanomas:
Superficial spreading melanoma (SSM): The superficial spreading melanoma is the most frequent form of black skin cancer. Symptoms: Flat, sometimes knotty skin changes, which are often sharply delineated from healthy skin. The colour can vary from brown, grey, pink to blue-black. Rarely some areas appear whitish. The SSM develops within one to four years, preferably on the back, chest and extremities.
Nodular melanoma (NM): The nodular melanoma is the most aggressive form of black skin cancer. Symptoms: Like SSM, nodular melanoma often develops on the back, chest and extremities. In the process, a raised, knotty and often bleeding tumour of blue to dark brown colour develops quickly (within a few months). It grows strongly into the deep. Therefore, this form of black skin cancer has the worst prognosis of all melanomas.
Lentigo maligna melanoma (LMM): Lentigo maligna melanoma develops slowly over years to decades on the ground of the precancerous stage Lentigo maligna. Especially older people suffer from this form of black skin cancer. Preferred locations include sun-exposed skin areas such as the face, neck, arms and hands.
Acrolentiginous melanoma (ALM): Of the four melanoma types mentioned here, ALM is the rarest form of black skin cancer. Symptoms: Acrolentiginous melanoma often forms blurred, multicoloured patches at the extremities (acra), i.e. in the area of the palms of the hands, soles of the feet, finger and toe ends, especially under the nails. It can be confused with a nail injury, nail fungus or a wart.
In addition to these main forms, there are also even rarer special forms of black skin cancer such as amelanotic melanoma (AMM) or choroidal melanoma.
Sting cell cancer: Symptoms
The appearance of prickle-cell cancer (squamous cell carcinoma, spinalioma) often resembles that of actinic keratosis in its initial stages. It often begins with a reddish-yellowish keratinization (hyperkeratosis), which usually cannot be removed without a small bleeding. The skin is often slightly reddened at the edges due to inflammation.
Advanced forms of spiny cell carcinoma turn whitish, become thicker and spread due to the increasing keratinization. Later symptoms of skin cancer are warty, tubercular skin growths which are firmly attached to the surface. They feel rough like rough sandpaper. If you try to remove these cornifications, the skin starts to bleed.
Spinaliomas are often found on the edge of the ears or on the face (also on the lips). They can occur on healthy skin as well as in scars or chronic wounds.
Basal cell cancer: Symptoms
Usually basal cell carcinomas (basaliomas) form in the so-called centrofacial area, i.e. in the face between the hairline and the upper lip. Often they are also found on an auricle, on the hairy scalp and in the lower third of the face. Somewhat less frequently basaliomas occur on the trunk, arms or legs. Basal cell carcinomas do not occur on the mucous membranes of the mouth and genitals, the palms of the hands and soles of the feet.
This form of white skin cancer is very diverse in its appearance. The beginning is usually only a few millimetres in size, shiny, translucent or waxy nodules (papules). In some cases the first telangiectasias are already visible on the surface. These are the finest blood vessels visible to the naked eye. A light bloody crust often forms on the papules by shaving or scratching. Over the course of months and years, the surface of the papule sinks in the middle – a hollow with a small pearl-like rim is created. This indicates that the tumor is growing. On the rim you can see the smallest blood vessels. Typically, this wound has not healed even after weeks: Alternately it heals and bleeds.
This nodular (nodular) basal cell carcinoma is the most common variant of basal cell cancer. Further manifestations are about:
- Superficial (superficial) basalioma: This type of basalioma is often overlooked because it is similar to inflammatory skin diseases such as psoriasis. It occurs most frequently on the trunk, arms and legs.
- Pigmented basal cell carcinoma: This type of basal cell carcinoma is strongly pigmented and therefore darkly discoloured. It can therefore be confused with black skin cancer (malignant melanoma).
- Sclerodermiform basalioma: The basal cell carcinoma looks like a yellowish deposit and is often difficult to distinguish from healthy skin. Sometimes this form reminds in appearance of scar tissue. Nodules are hardly visible.
- Exulcerative growing basal cell carcinoma: In the face there is often an ulcerous decay of the basal cell carcinoma. If deeper tissue layers are destroyed, physicians speak of a destructively growing basal cell carcinoma.
Detect skin cancer: Tips
The skin is constantly changing. Spots and other changes are also formed again and again. Only very rarely is it actually skin cancer. Signs of a malignant skin tumour can also easily be confused with harmless changes. You should therefore ask your family doctor or a dermatologist to explain to you which symptoms skin cancer typically causes and how you can recognise them. After examining your skin, the doctor may also draw your attention to moles that you should keep an eye on, as they may develop into skin cancer. You can also look at pictures of skin cancer cases in books and on the Internet. This helps you to better assess skin changes in yourself.
Skin cancer: types of cancer
Roughly, three groups of skin cancer can be distinguished: white skin cancer, black skin cancer and some rare forms of skin cancer (such as Kaposi’s sarcoma, Merkel cell carcinoma and Dermatofibrosarcoma protuberans).
The white skin cancer
The term “white skin cancer” (or “light skin cancer”) is used to describe various forms of skin cancer: Basal cell carcinoma (basal cell carcinoma, basal cell carcinoma) and prickle cell carcinoma (prickle cell carcinoma, spinalioma or squamous cell carcinoma). An early form of prickle-cell cancer is actinic keratosis.
White skin cancer is by far the most common form of malignant skin tumors. It is less dangerous than malignant melanoma because, unlike malignant melanoma, it forms no or hardly any metastases in other parts of the body. White skin cancer can therefore usually be completely removed and is rarely fatal.
You can read more about white skin cancer and its main representative – the basal cell carcinoma – in the article White skin cancer.
Sting cell or squamous cell carcinoma
Spinal cell carcinoma (spinalioma, squamous cell carcinoma) mainly affects people over 60 years of age. Mostly affected are parts of the body that are frequently exposed to the sun. These are for example face, ears, back of the hand and forearms.
Squamous cell carcinoma grows more aggressively than basal cell carcinoma: the malignant tumor successively destroys the surrounding tissue. If not detected and treated early, it can cause metastases in other parts of the body. This then makes treatment more difficult and worsens the prognosis. About 40 to 50 out of 1,000 patients die from this form of skin cancer (for comparison: basal cell cancer is fatal in only about one out of 1,000 patients).
You can read everything important about the causes, symptoms, treatment and prognosis of spinalioma in the supplement Squamous cell carcinoma.
Actinic keratosis
Like Bowen’s disease (Morbus Bowen), actinic keratosis is a possible precursor of sting cell cancer. It is accompanied by sharply defined redness, which feels like fine sandpaper when touched. These skin areas can also cornify later. Sometimes they remain inconspicuous for years or even for life. But it can also develop into a sting cell carcinoma.
Whether that happens or not cannot be predicted. To be on the safe side, actinic keratosis should therefore always be treated. For example, the skin changes can be removed surgically, “frozen” with liquid nitrogen, removed by laser or caustic solutions or treated with a special cream/ompany ointment.
You can read more about this widespread early form of sting cell cancer in the article Actinic keratosis.
Malignant melanoma
Black skin cancer (malignant melanoma) can develop on all skin areas of the body – even those that are hardly ever exposed to the sun (such as the genital area, hairy scalp, sole of the foot, under the nails). It is clearly rarer than white skin cancer: altogether about 328 of 100,000 people fall ill with skin cancer every year. Approximately 290 of them are diagnosed with “white skin cancer”. The remaining 38 or so patients have malignant melanoma. The mean age of onset of the disease is 64 years (men) and 58 years (women).
In spite of its lower incidence, black skin cancer is much more feared than white skin cancer. This is because it is more aggressive and spreads much faster throughout the body. The exact course of the disease depends, among other things, on the type of malignant melanoma. The different types of melanoma differ in their aggressiveness.
You can read everything important about causes, symptoms, diagnosis, therapy and prognosis of malignant melanoma in the article Malignant melanoma.
Kaposi’s Sarcoma
Kaposi’s sarcoma is a rare form of skin cancer that can also affect mucous membranes and internal organs. It occurs in different variants. For example, in addition to the classic form of the disease, there is HIV-associated Kaposi’s sarcoma: it develops in people whose immune system is weakened due to HIV infection.
This type of skin cancer is also often observed in patients whose immune system has to be suppressed for medical reasons (iatrogenic immunosuppression). This is necessary after an organ transplant, for example. The fourth disease variant is the so-called endemic Kaposi’s sarcoma. In tropical Africa it occurs mainly in children and young adults.
The different disease variants differ in their aggressiveness and treatment. You can read more about this in the article Kaposi’s Sarcoma.
Skin cancer: treatment
How the skin cancer therapy looks like in individual cases depends on several factors. The type of skin cancer and how advanced the tumor is, plays a major role. The patient’s age and general state of health are also taken into account when planning therapy.
White skin cancer: treatment
For the treatment of the two forms of white skin cancer, basal cell carcinoma and spinalioma, different procedures are available. The best chance of success is surgery. If this standard therapy is not possible or insufficient, other methods of skin cancer treatment may be considered alternatively or additionally (radiotherapy, photodynamic therapy etc.).
Operation
During the operation, the surgeon removes the cancerous tumour as completely as possible – together with a seam of apparently healthy tissue around it. This increases the chance that all cancer cells will be “caught”. To verify this, the removed piece of skin is examined under the microscope for fine tissue (histological). If suspicious cell alterations are found in the supposedly healthy border area despite everything, another operation must be performed and further skin tissue must be cut out. This is repeated until the tissue removed proves to be really healthy under the microscope.
This procedure in the surgical treatment of skin cancer is called microscopic controlled surgery or micrographic surgery. It is intended to ensure that all cancer cells around the tumor site have been “caught”.
In the case of a very deep basalioma or spinalioma, so much tissue must be removed that the result often leads to cosmetic problems. Then, after completion of the skin cancer treatment, some skin from another part of the body can be transplanted to this site (skin transplantation).
In the case of very superficial basaliomas or spinaliomas, it is often sufficient to scrape out the cancer cells to a certain extent (curettage). This means that the doctor scrapes out the diseased tissue with a special medical instrument.
In certain cases, so-called cryosurgery (cryotherapy) is also possible as skin cancer therapy. In this procedure, the changed skin areas are treated with liquid nitrogen for a short time (“frozen”). Ice crystals form inside the cells, which destroy the cells. The method is used, for example, for sting cell cancer and its preliminary stage (actinic keratosis).
Radiotherapy
Skin cancer irradiation by means of radiation (radiotherapy) is mainly used if the tumour is very large or unfavourably located (approximately near the eye). Even in older patients for whom surgery would be too stressful, a basalioma or spinalioma can be irradiated instead.
In most cases, very high-energy X-rays are directed at the tumor in several sessions, which causes the cancer cells to die. The attending physician focuses the rays as precisely as possible on the tumor in order to minimize the risk to surrounding healthy tissue.
Photodynamic therapy (PDT)
Photodynamic therapy (PDT) can also be considered for superficial basal cell cancer (basalioma) and actinic keratosis. Here, the altered skin areas are first treated with a special drug that makes the tissue more light-sensitive. The area is then irradiated with very long-wave light (no X-rays). It makes the tumor cells die.
Sunbathing must be avoided during the time of photodynamic therapy!
Chemotherapy
Sometimes white skin cancer is also treated with chemotherapy (outpatient or inpatient). Patients receive special drugs that inhibit the division and proliferation of cancer cells (cytostatics).
In systemic chemotherapy, the cytostatic drugs are administered internally (e.g. as tablets or infusions) so that they can take effect throughout the body. This form of skin cancer treatment is used for basal cell cancer if the tumour cannot be operated on or if there are several tumours. In the case of squamous cell carcinoma (spinalioma) it may be necessary if the tumour is inoperable or has already formed metastases. In this case, chemotherapy can possibly be combined with radiation.
In local chemotherapy, the cytostatic drugs are applied as an ointment directly at the site of the tumour. The effect of this skin cancer treatment is therefore locally limited (in contrast to systemic chemotherapy). On the other hand, the risk of side effects is lower. Local chemotherapy can be used for superficial basal cell carcinoma and actinic keratosis.
Immunotherapy
Immunotherapy (immunomodulating therapy) is a newer possibility of skin cancer treatment in certain cases of basalioma or actinic keratosis. A cream containing the active ingredient imiquimod is regularly applied to the affected skin areas over several weeks. Imiquimod activates the skin’s immune system, which then attacks the tumour cells in a targeted manner. Visible tumour areas as well as those not yet visible to the naked eye are removed without pain. Scars are not left behind with this skin cancer therapy. Since long-term results are still pending, it cannot be ruled out that higher relapse rates than with surgical therapy will occur.
Black skin cancer: treatment
Even more so than in the case of white skin cancer, the treatment of malignant melanoma is oriented to the tumor stage. Malignant melanoma forms metastases at an early stage. A total of five melanoma stages (partly with subgroups) are distinguished. The scale ranges from stage 0 (= superficial, limited tumour without metastases) to stage IV (= tumour that has already formed metastases in other organs).
Operation
Surgery is the therapy of choice in all stages of black skin cancer. The tumour is removed as completely as possible with a seam of healthy tissue. How deep the incision is made into healthy tissue depends on the size of the tumour.
If the melanoma is more than one millimeter in diameter, a tissue sample is also taken from the sentinel lymph node. This is the lymph node that is closest to the tumor in the lymphatic drainage area. He is being examined for cancer cells. As soon as individual cancer cells detach from the melanoma and spread throughout the body, the sentinel lymph node is usually the first to be affected. If this is indeed the case, it is removed – usually together with neighbouring lymph nodes. In addition, further treatments are then usually recommended to support the success of the therapy. This can be immunotherapy with interferon (interferon therapy), radiotherapy or chemotherapy, for example.
Interferon therapy
The active ingredient interferon-alpha can influence the immune system in such a way that it supports skin cancer treatment: Administered as an injection, it activates certain immune cells (killer cells) which attack and destroy the cancer cells. Interferon treatment is often used when the malignant melanoma has exceeded a certain size or has already metastasized: After surgical removal of all visible growths, interferon therapy can eliminate any micrometastases (invisible metastases). This should increase the chances of recovery.
Radiotherapy and chemotherapy
In the case of more advanced black skin cancer, radiotherapy may follow the operation. Affected lymph nodes and metastases in distant organs can be treated in this way. Radiation therapy can also be useful if the malignant tumour cannot be completely removed during the operation.
Radiation can also be used as a substitute for surgery: If, for example, the patient is too old for the operation or the tumour is inoperable, irradiation is often used instead.
Occasionally, surgical skin cancer treatment is supported by chemotherapy: The cancer drugs (cytostatics) administered are designed to eliminate distant metastases.
Targeted therapy
A new possibility of skin cancer therapy for advanced malignant melanoma is the administration of drugs that act specifically against cancer cells: The active substances contained (such as dabrafenib) can inhibit the proliferation of cancer cells and thus reduce the size of the tumour. However, this only works if the cancer cells have a specific genetic change. This must therefore be clarified in advance.
Targeted therapies have a major advantage: conventional treatment methods such as chemo- or radiotherapy cannot distinguish between healthy cells and cancer cells. This means that healthy cells are also damaged, which causes corresponding side effects (hair loss etc.). In contrast, targeted therapies are only directed against selected targets of cancer cells. Healthy cells are therefore spared.
Rare forms of skin cancer: treatment
There is no generally accepted standard treatment regimen for Kaposi’s sarcoma. Individual factors as well as the variant of the disease are taken into account when planning therapy. For example, in classic Kaposi sarcoma, radiation therapy is usually sufficient to remove the tumor. In individual cases, however, chemotherapy is also carried out, for example if the tumour is very large. There is also the possibility of immunotherapy with interferons.
In HIV-associated Kaposi’s sarcoma, the administration of HIV drugs (as combined antiretroviral therapy, cART) plays an important role: In patients who have not yet been treated with cART when the skin cancer occurs, the tumour often stops growing as soon as the HIV drugs are started. Sometimes the Kaposi syndrome even disappears completely. If the skin cancer only develops during HIV treatment, this must be tested for its effectiveness. In advanced skin cancer sera, antiretroviral treatment is combined with chemotherapy.
Kaposi’s sarcoma, which develops when the immune system is suppressed by medication, often regresses on its own as soon as the medication (immunosuppressants) is discontinued. If this is not possible, it may be sufficient to reduce the dose of the preparations. In addition, the tumour can be irradiated.
The Merkel cell carcinoma is usually removed surgically. Subsequently, the tumour area and the neighbouring lymph nodes should be irradiated. Chemotherapy can also be effective for this form of skin cancer.
Dermatofibrosarcoma protuberans (DFSP) is also operated on whenever possible: The tumour is cut out together with a safety margin (i.e. together with a seam of demonstrably healthy tissue). If an operation is not possible, skin cancer treatment is often carried out by means of radiation. A more recent treatment option for DFSP is a targeted therapy with imatinib. This active ingredient inhibits tumour growth. However, it is only used in certain cases, such as when the tumour is inoperable or has already progressed far or is returning after a successful initial treatment.
Skin cancer: causes and risk factors
The main cause of skin cancer is UV light. In addition, other risk factors are now known. However, the exact mechanism of carcinogenesis has not yet been clarified in part.
White skin cancer: causes
If the skin is repeatedly exposed to ultraviolet (UV) light, the risk of white skin cancer increases. This does not apply to the UV rays in sunlight as well as in the solarium. Skin cancer is a possible late consequence in both cases. In addition to the solarium, other artificial UV sources also carry a risk of skin cancer. These include UV devices for phototherapy (e.g. for neurodermatitis or psoriasis) or for curing plastic (nail studio, dentist).
UV light is electromagnetic radiation with a wavelength of 100 to 400 nanometres (nm). Strictly speaking, there are three different types of UV rays:
- UV-A: Wavelength between 315 and 400 nm; tans the skin in the solarium and causes the skin to age prematurely.
- UV-B: Wavelength between 280 and 315 nm; tans the skin in sunlight
- UV-C: Wavelength between 100 and 280 nm; is almost completely filtered out of sunlight by the ozone layer.
Tanning is caused by the fact that the skin increasingly produces the brown dye (pigment) melanin – as protection against the high-energy UV rays. If the irradiation is too strong, burn symptoms such as reddening and pain (sunburn) occur.
But even without these visible consequences, UV radiation damages the skin, more precisely the genetic material of the skin cells. If the cells fail to repair this damage, they can degenerate and become cancer cells. This can also only happen years or decades after repeated or intensive exposure to the sun – the skin never forgets UV damage and sunburn!
Skin cancer: particularly light skin types at risk
How much sun a person can tolerate well varies greatly. The lighter the skin type, the less self-protection the skin has, as less melanin (skin pigment) is produced. we can roughly divide it into four skin types, so the classification can be better understood:
- Skin type I: Sunburn develops very quickly. Solar radiation hardly ever leads to a tan (“Celtic type”).
- Skin type II: Sunburn is frequent, tanning is slow (“light-skinned European type”).
- Skin type III: Sunburn is only occasional, tanning works well (“dark skinned European type”).
- Skin type IV: Sunburn is very rare, a good tan is present even without significant sun exposure (“Mediterranean type”).
Other causes of white skin cancer
Repeated, unprotected UV exposure is the most important cause of basal cell cancer and sting cell cancer. In addition, other factors can also promote the development of white skin cancer:
In some families basal cell cancer is more common. So there is apparently a genetic predisposition for this type of skin cancer. Both basal cell cancer and sting cell cancer can be promoted by contact with various substances and chemicals such as arsenic and by-products of oil processing. There are also some hereditary diseases that increase the risk of white skin cancer (such as xeroderma pigmentosum).
People with a weakened immune system are also more susceptible to white skin cancer. If, for example, the immune system has to be suppressed by medication after an organ transplant, the risk of skin cancer increases.
White skin cancer rarely develops as a result of chronic wounds or scars (such as burn scars).
Black skin cancer: causes
The most important cause of black skin cancer is also UV light: repeated sunburns (especially in childhood) can cause malignant melanoma. There is also a certain hereditary predisposition for this dangerous form of skin cancer. This is supported by the increased occurrence of black skin cancer in some families. The light skin types I and II are significantly more frequently affected by black skin cancer.
In addition, there are some risk factors for malignant melanoma that also play a role in white skin cancer. These include some hereditary diseases (such as xeroderma pigmentosum) and a weakened immune system (for example, after organ transplantation due to taking medication to inhibit the immune system).
People with a previous melanoma also bear an increased risk of disease: such a return of the black skin cancer is usually observed in the first five years after the removal of the first tumour.
The risk of malignant melanoma is also slightly increased among airline personnel.
Black skin cancer & birthmark / liver spot
In some cases, skin cancer of the malignant melanoma type (black skin cancer) develops from a mole or birthmark. One should keep an eye on a mole or birthmark especially if someone has a lot of them: Anyone who has more than 40 or 50 such pigmentation marks should have them regularly examined by a dermatologist.
In most cases, however, malignant melanoma develops “out of nowhere”, i.e. on normal skin without pigmentation marks.
A birthmark (nevus) is a benign, light or dark skin growth that is congenital or acquired. A liver spot (pigment nevus) is a brown skin change that develops from pigment-forming skin cells (melanocytes). Colloquially, however, birthmark and mole are used synonymously (as terms with the same meaning).
Rare forms of skin cancer: causes
UV radiation has little or no significance for the development of Kaposi’s sarcoma. The same applies to Merkel cell carcinoma and Dermatofibrosarcoma protuberans (DFSP). Other risk factors play a role in these very rare forms of skin cancer:
Thus, certain herpes viruses are involved in the occurrence of Kaposi’s sarcoma (human herpes virus 8, HHV-8). However, infection with these viruses alone cannot cause skin cancer. Rather, other factors must be added (such as genetic factors).
The exact causes of Merkel cell carcinoma are unclear. However, certain viruses also appear to be involved in the development of cancer.
How it can come to a Dermatofibrosarcoma protuberans is not known. So far, no risk factors for this type of skin cancer are known.
Why is skin cancer increasing?
The World Health Organization (WHO) estimates that every year two to three million people worldwide are newly diagnosed with white skin cancer and 250,000 with black skin cancer. At the same time, the number of illnesses has been rising for decades. This is probably due to an overly careless handling of UV radiation, for example when sunbathing or in solariums. Above all, intensive sun exposure and sunburn in childhood significantly increase the risk of skin cancer.
Skin cancer: examinations and diagnosis
Some people shy away from going to the doctor. However, as with hardly any other type of cancer, it is decisive for the prognosis of skin cancer how early the tumour is discovered and treated. If you discover a conspicuous area of skin on you, you should therefore have it checked by your dermatologist. He can determine whether it is really skin cancer.
Collection of the medical history
First of all, the doctor will take your medical history in consultation with you (anamnesis). He inquires about any skin changes discovered, possible complaints and possible previous illnesses. Common questions are about:
- What complaints do you have?
- When did you first notice the suspicious skin area?
- Is the noticeable area bleeding or itching?
- What medications are you taking?
- Are there or have there been similar complaints in your family, for example with parents, siblings or children?
- Are you familiar with any skin diseases such as psoriasis?
- Do you spend a lot of time in the sun, privately or for professional reasons?
- Do you go to the solarium regularly?
Studies
In the next step, the dermatologist examines the conspicuous skin area thoroughly with an incident light microscope (dermatoscope). He may also want to look at the rest of the skin to check for any abnormalities.
If the dermatologist suspects skin cancer, he will arrange for further examinations. This includes, above all, the removal of a tissue sample: the suspicious skin area is removed under local anaesthetic, together with a safety margin. The tissue is examined in detail (histologically) by a pathologist in the laboratory. In this way it can be determined whether skin cancer is actually present. In this case, further investigations will follow:
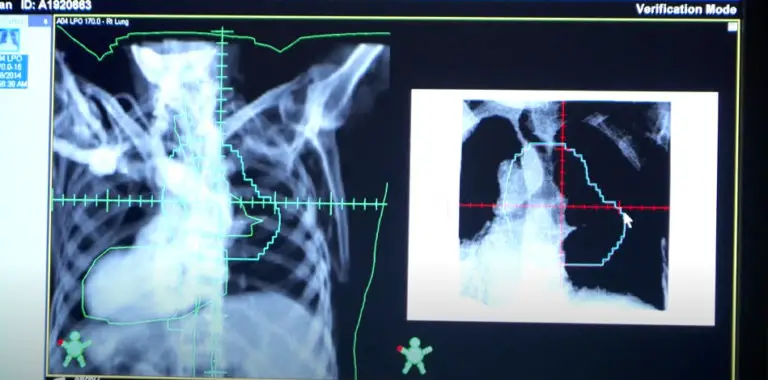
- Imaging procedures such as X-rays, computer tomography (CT), magnetic resonance imaging (MRI) or ultrasound (sonography) can show whether and how far the cancer has already spread in the body (metastasis). This is very important for choosing the right therapy.
- Blood tests tell us something about the general condition of the patient and the function of important organs in the body. This is important, among other things, in order to be able to estimate the risk of anaesthesia (during the operation).
- The skeletal scintigraphy (bone scintigraphy) is a nuclear medical examination that can be used to detect bone metastases.
Skin cancer screening (early detection)
The statutory health insurance funds pay all insured persons from the age of 35 years every two years for an examination for early detection of skin cancer (skin cancer screening). A specially trained doctor examines the entire skin surface. The aim of skin cancer prevention is to detect malignant changes in the skin at an early stage. Then the chances of recovery are almost 100 percent.
A doctor receives approval for skin cancer screening by participating in a special training program. Skin cancer screening is therefore usually performed by general practitioners with appropriate training or by dermatologists.
How does the skin cancer screening work?
The skin cancer screening is completely painless. The doctor will examine your skin over your entire body (including your scalp) for suspicious changes.
If the general practitioner is not quite sure about a skin area, he will refer you to a dermatologist for safety reasons. He’s gonna repeat the skin cancer screening. However, this is not a cause for concern, as the dermatologist usually gives the all-clear.
The dermatologist takes a closer look at conspicuous skin areas with a special magnifying glass (dermatoscope). If skin cancer is suspected, he may take a tissue sample (biopsy) or completely remove the conspicuous skin area under local anaesthetic and send it to a laboratory. The careful examination of the tissue brings certainty as to whether it really is skin cancer. Very often, however, it turns out to be just a harmless skin change.
The skin cancer screening also includes a consultation on the danger of UV radiation (sun, solariums).
Own contribution to skin cancer screening
Skin cancer and its precursors can often be detected without the need for expensive equipment. Every layman can contribute to this. It is decisive for the own skin cancer early detection to examine the skin regularly for changes. The skin can only be examined well if you can see it clearly. The examination should therefore take place in a bright, well lit room.
One should pay particular attention to those areas of the skin on which the sun shines, as skin cancer is much more common here. On parts of the body such as the back, a mirror or examination by a friend or partner can be helpful. It is particularly important in the early detection of skin cancer to pay attention to changes that could indicate black skin cancer, as this is particularly dangerous. Of all things, this dangerous cancer often occurs on parts of the body that are only rarely exposed to sunlight.
How can you recognize a malignant melanoma?
The so-called ABCD rule can be helpful in the early detection of black skin cancer. It serves as an orientation for the assessment of dark skin spots (birthmark, pigment mark):
A (asymmetry): If a dark skin patch is not round or oval but asymmetric, it should be examined by a doctor.
B (Limit): A birthmark is usually sharply delineated from the surrounding skin. If, on the other hand, the stain has runners into the surrounding skin or appears blurred, washed out, it could possibly be caused by skin cancer.
C (Colour): If a skin spot has different colour tones (for example light brown and deep black), this is conspicuous. A skin cancer screening provides certainty.
D (diameter): Every birthmark that is more than two millimetres in diameter must be observed.
When should you see a doctor?
The self-examination is very important for the early detection of skin cancer. In case of doubt, you should see your doctor as soon as possible. In the following situations a visit to the doctor is highly recommended:
- According to the criteria of the ABCD rule, a pigment spot is conspicuous or changes in shape, colour or size.
- A pigmentation mark begins to burn, itch or bleed.
- Rough skin areas or crusts are formed. This may indicate white skin cancer. Special attention should be paid to sun-exposed areas (face, back of the hands, etc.).
- If you have an above-average number (more than 40) of pigment spots (moles), these should always be examined regularly.
- You will notice white spots on the edge of the tongue or in the oral mucosa.
Skin cancer: course of disease and prognosis
The course of the disease depends, among other things, on the type of skin cancer. While some tumours grow only slowly, others spread quickly and form metastases early on. This makes the treatment of skin cancer more difficult. The chances of cure also deteriorate with the growth and spread of the tumour. In general, the following applies: The chances of healing skin cancer are better the earlier the malignant tumour is discovered and treated. In the following you will find more detailed information on the course of the most important forms of skin cancer, chances of cure and prognosis.
Basal cell cancer
Basal cell cancer grows only slowly. In addition, it rarely causes metastases in other organs. This also applies in advanced tumour stages, when large areas of skin (for example the entire nose) have been destroyed by the cancer. Overall, the basal cell carcinoma therefore has a good prognosis: it is easily treatable, so that up to 95 percent of patients will be completely healthy again. Deaths are rare: Only about one in 1,000 patients dies of cancer.
Risk of relapse: Regular follow-up examinations after completion of treatment are very important. More than four out of ten patients develop further basaliomas within the first three years after initial diagnosis. If these new tumours are carefully monitored, they can be detected and treated early. The intervals at which the follow-up examinations are sensible depend on the individual case. The attending physician will suggest suitable appointments for each patient. Experts currently recommend that this aftercare should not be limited in time.
Sting cell cancer
Spiked cell carcinoma grows more aggressively than basal cell carcinoma. It gradually destroys the surrounding tissue. Untreated, a spinalioma can spread throughout the body and form metastases in lymph nodes and other organs. This influences the prognosis: If sting cell cancer is discovered before it has metastasized, it is usually easily treatable. As soon as daughter resettlements occur, the chances of recovery decrease. Statistically speaking, cancer ends fatally in 40 to 50 out of 1,000 patients.
Risk of relapse: As with basal cell carcinoma, regular check-ups are recommended for spinalioma after completion of therapy (for at least five years). About half of those affected develop a new tumour within five years of the initial diagnosis.
Malignant melanoma
The different types of black skin cancer show different courses: Some melanoma types grow on the skin surface for a longer time and can therefore be treated quite well. Other types penetrate quickly into deeper tissue layers and soon spread throughout the body via the blood and lymphatic system. Thus metastases form at an early stage. The affected patients can die within a few months if left untreated.
Apart from the melanoma type, the tumor stage at the time of diagnosis also influences the chances of cure. In Germany, more than half of all malignant melanomas are detected at an early stage. Almost all of the affected patients can be cured. However, the later black skin cancer is discovered and treated, the worse the chances of recovery and the higher the risk of death. In general, 15 to 20 out of 100 male patients and 10 to 15 out of 100 female patients die within ten years after the diagnosis of malignant melanoma.
Risk of relapse: Anyone who has already been diagnosed with malignant melanoma has an increased risk of developing a dangerous melanoma again (secondary tumor). That is why regular check-ups after completion of the treatment are very important. This follow-up care for malignant melanoma should last for ten years.