Thrombosis: symptoms, treatment, causes, prevention
Thrombosis: symptoms, treatment, causes, prevention
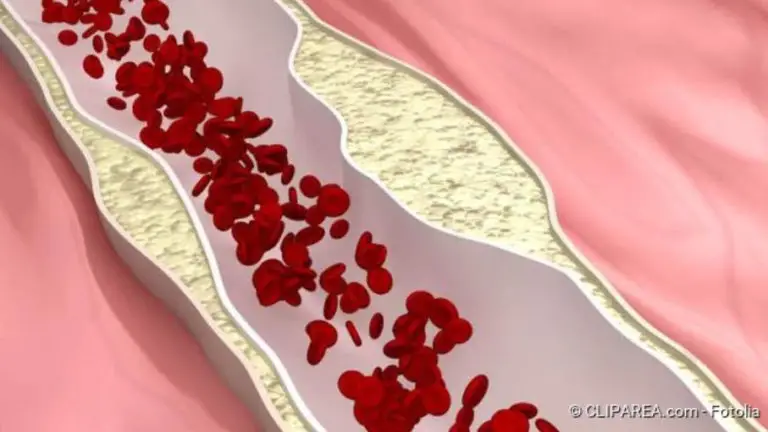
Thrombosis is a vascular occlusion caused by a blood clot (Source). The most common form of thrombosis is in the veins in the leg (Source). Important signs of thrombosis are swelling, pain, (Source) and a red or bluish discoloration of the skin Fever is also possible (Source). A thrombosis is dangerous because the clot can become loose and be flushed into other organs (Source). Read all important information about thrombosis symptoms, treatment, and prevention!

Thrombosis: Brief overview
- Most frequent localizations: Legs (especially lower legs), pelvic area, arms, upper or lower vena cava (Source)
- Typical symptoms: swelling, redness, overheating, pain and feeling of tension, fever, accelerated pulse (Source)
- Treatment: Compression bandage or compression stockings, elevation, anticoagulant medication, thrombectomy (OP)
- Important research: Ultrasound image, phlebography (“vein x-ray”), CT, blood test (D-dimers, coagulation factors)
- Dangers: Pulmonary embolism (pulmonary artery occlusion), vascular and tissue damage (postthrombotic syndrome)
- Special form: Analthrombosis (anal venous thrombosis)
Symptoms of thrombosis
There are a number of very typical signs of thrombosis. Depending on where the clot has formed, the symptoms may differ in part.
The most common form of thrombosis is in the veins in the leg. The signs of this may be slight or absent. Typical are pain on the occurrence, when stretching the calf as well as pressure on the calf and sole of the foot. With pronounced thromboses, the leg sometimes swells or shows a bluish-red discoloration. Sometimes dilated veins in the groin and lower abdomen are also visible.
Let your internist determine your individual thrombosis risk. Patients at risk should wear thrombosis stockings and avoid the pill. The risk of thrombosis is also increased on long-haul flights, after orthopedic operations, and with bedridden persons, so make sure you get enough exercise. And in the case of acute leg complaints, a doctor should clarify the cause as quickly as possible.
The greatest danger is that a piece of the blood clot comes loose, gets into the lung blood vessels, and closes them. The so-called pulmonary embolism manifests itself by a rapid pulse, shortness of breath or shortness of breath, and sometimes dizziness. These symptoms indicate a dangerous emergency and must be treated immediately. Because a pulmonary embolism can be fatal.
Symptoms of thrombosis in the leg
Thromboses form particularly frequently in the large veins of the lower leg. This is because there the blood flows back to the heart particularly slowly against the force of gravity. The most common signs of thrombosis are then:
- Swelling of the calf, often also of the ankle region and foot
- Feeling of heaviness and tension in the lower leg
- Pain in the lower leg, sometimes also in the foot, thigh or groin, which can resemble a sore muscle
- tense (shiny) and bluish discolored skin
- Overheating of the lower leg
- more visible skin veins (so-called warning veins)
- mild fever
- accelerated pulse
Thromboses in the arms usually cause more severe symptoms than vascular occlusions in the legs. In addition, they are noticeable by an increased vein pattern, because the blood seeks its way to the heart via detours.
Even if some of the symptoms mentioned are missing, thrombosis in the leg cannot be ruled out. Neither is the thrombosis signs mentioned any more proof that leg vein thrombosis really exists.
In thrombosis, a blood clot forms in a blood vessel and blocks it. Usually, a vein in the leg is affected.
Symptoms of thrombosis in the arm
The veins in the arm can also be blocked by blood clots. This occurs much less frequently overall than in the leg. Typical thrombosis symptoms in the arm are:
- Swelling and overheating of the affected arm
- Swelling of the hand
- bluish protuberant skin veins
- partial reddish-purple discoloration of the arm
- Pain with pressure on the arm and when moving
In principle, thromboses can occur in all blood vessels of the body. In contrast to thromboses in the extremities, the symptoms are often ambiguous. Severe pain or dysfunction of organs may occur. To clarify such unspecific thrombosis symptoms further medical examinations are always necessary.
Symptoms of an anal thrombosis (anal venous thrombosis)
An anal thrombosis is noticeable by a painful swelling in the anal area. Analthrombosis is often difficult to distinguish from so-called hemorrhoids. However, it has another cause: In an analthrombosis, the blood clot is formed in a small vein of the lower anal canal. The painful hemorrhoid, on the other hand, is an enlarged blood vessel of an arteriovenous vascular cushion which penetrates from the inner anal canal to the outside.
Anal venous thromboses are very painful, especially because they are directly in the area of the opening. Analthrombosis can usually be treated well, however. Here you can learn more about the symptoms, causes, and therapy of analthrombosis!
Thrombosis treatment
A thrombosis can be treated by medication, compression therapy, or surgery. Which method is used depends, among other things, on where the clot has formed. Often, however, the different treatment approaches must be combined.
The most important goal of thrombosis treatment is to prevent the clot from separating from the vein wall and migrating with the bloodstream to vital organs. This is because there is then a risk of a so-called embolism (for example a pulmonary embolism), i.e. the clogging of an artery by the clot with potentially life-threatening consequences. In addition, long-term, irreparable damage to the affected blood vessels, extremities, or organs (postthrombotic syndrome) should be avoided.
High storage and compression
Important immediate measures in the case of a freshly occurring thrombosis in the extremities consist of raising the affected leg or arm and applying a compression bandage. This can prevent the blood from accumulating even more and the limb from swelling further.
The compression bandage must extend well beyond the site of the thrombosis – in the case of a lower leg thrombosis, that is, to below the knee. It must be tight to compress the veins so strongly that the blood flows better in them. But he must not constrict the limb at any point.
A good way to achieve a sufficiently strong and even degree of compression is to use thrombosis stockings of compression class II. Compression treatment should be continued in the long term if veins have been damaged by the thrombosis.
Thrombosis treatment with medication
Drug treatment of thrombosis is intended to prevent the blood clot from growing further and possibly being washed into the pulmonary arteries. In the best case, the medication can cause the body’s own substances (enzymes) to reduce the size of the thrombus again or even dissolve it completely. In addition, anticoagulant drugs can prevent the new development of thrombosis.
Acute treatment of thrombosis
One starts the treatment of thrombosis with a so-called initial anticoagulation, which should start immediately if the diagnosis of thrombosis has been made or if thrombosis is very likely the cause of symptoms.
The drug heparin, which inhibits blood clotting, is usually used for this purpose. For this purpose, heparin must be given in high dosages as a syringe under the skin (subcutaneous injection) or as an infusion. This is because the drug would decompose in the gastrointestinal tract and then not enter the bloodstream.
The active ingredient Fondaparinux is also injected under the skin. It is mainly used when patients have previously reacted to hepar administration with a life-threatening drop in the number of blood clotting platelets (thrombocytes). Other active ingredients in the treatment of acute thrombosis are the so-called DOACs (direct oral anticoagulants) rivaroxaban and apixaban.
Long term treatment after thrombosis
Subsequently – usually after about five to ten days – patients receive an anticoagulant drug in tablet form to prevent a new clot from forming. This so-called maintenance therapy is continued for three to six months. So-called vitamin K antagonists are used for this purpose. These are counterparts of vitamin K, which is important for blood coagulation. The active ingredients phenprocoumon and warfarin are used in Germany in particular.
Important: The correct dosage of these drugs must be checked regularly by blood tests of the so-called coagulation values!
Surgical thrombosis treatment
Especially for young patients, who are experiencing thrombosis in a large vein in the leg-pelvic area for the first time, surgery may be the best treatment option. The aim is to grasp the clot (thrombus) with a catheter and pull it out of the vein. Doctors also speak of “recanalizing” because the procedure makes a blocked blood vessel pass through again. The doctors also check if there is an obstruction in the vein that can be removed.
Often a thrombus-dissolving medication is also given via the catheter. This local form of thrombosis treatment has better success rates and lower risks than the systemic treatment frequently used in the past, in which the drug had to be distributed throughout the body in high doses.
Recanalization therapy should be performed as early as possible to reduce the risk of postthrombotic syndrome. Possible complications of this type of thrombosis therapy are bleeding, but also accidental separation of parts of the clot. These could then move further in the venous tract towards the heart and the pulmonary circulation.
In individual cases, patients with leg vein thrombosis have a kind of “sieve” implanted into the vena cava (vena cava filter), either permanently or temporarily. It is intended to prevent detached blood clots from being washed into the lungs. This procedure is suitable for patients who repeatedly suffer a pulmonary embolism despite taking anticoagulant medication.
Thrombosis: Causes And Risk Factors
Thromboses are blood clots that form in the blood vessels – almost always in veins. They can basically have three different causes, which can exist alone or in combination:
- Flow obstacles in the blood vessel: damage/illnesses or deposits on the vessel wall or constrictions of the blood vessels due to mechanical pressure from outside (e.g. scarring, tumors)
- slow flow rate: in pathologically dilated veins (varicose veins), due to the effect of gravity and/or insufficient muscle tension (in cases of immobility, paralysis or after operations), lack of fluid (blood becomes thicker)
- increased blood coagulation: diseases of the blood coagulation system, severe systemic diseases (cancer, autoimmune diseases), side effects of medication (e.g. from the “pill”), smoking
Travel thrombosis and thrombosis after operations
The blood return to the heart must work against gravity in the deep veins of the legs. This is supported by two mechanisms in healthy, physically active people:
- Venous valves: They act like valves and only allow blood to flow in one direction, namely to the heart.
- Muscle pump (muscle-vein pump): Due to the work of the (calf) muscles, the veins in the leg are repeatedly compressed briefly. In cooperation with the venous valves, the blood is thus pressed towards the heart.
If one or both mechanisms do not work, the blood flow can be severely slowed down and the risk of thrombosis increases. This is the case, for example, when sitting in a car, train, or plane for a long time. This is why it is often referred to as “travel thrombosis”. But sitting at the computer for hours on end can also increase the risk of thrombosis.
Similarly, after injuries or operations, after which the leg must be immobilized or generally strict bed rest must be maintained, the natural action of the muscle pump is no longer required. Since every trauma – and this includes operations in a broader sense – also significantly increases the blood’s readiness to coagulate, the risk of thrombosis after operations is greatly increased.
Thrombosis in varicose veins
Varicose veins (varices) are strongly dilated blood vessels. They occur particularly frequently in the area of the legs, especially the lower legs. In varicose veins, the blood flows more slowly and in addition, the natural valves in the veins, the venous valves, no longer function properly. This also increases the risk of thrombosis.
Thrombosis: Diagnosis And Examination
In the case of a venous thrombosis in one leg, the leg is overheated and swollen. Certain pressure points and movements trigger pain, which the doctor (usually a specialist in internal medicine) can determine with a physical examination. Typical are for example:
- Calf pain when the tip of the foot is raised (Homans sign)
- Pain when pressing the calf (Meyer’s sign)
- Pressure pain on the inside of the foot (Payr sign)
In addition, an ultrasound examination can provide an image of the occlusion of veins. In general, superficial thrombosis is characterized by more severe symptoms and is therefore often easier to diagnose than vascular occlusion in deeper veins (phlebothrombosis). However, the latter often has serious consequences.
With a phlebography (also: phlebography) the blood vessels in the body can be depicted on an X-ray. The procedure is therefore well suited for the diagnosis of deep vein thrombosis. A contrast medium is injected into a superficial vein on the back of the foot. To ensure that the contrast medium finds its way into the deep leg veins, the veins near the skin surface are first tied off with a moderately tight bandage. Where thrombosis exists, the flow of the contrast medium is interrupted or appears “constricted”.
A much-used examination method in vascular medicine is computer tomography (CT). In this procedure, the patient’s body is virtually cut into slices using X-rays. Due to the high image density, vessels and organs can also be displayed. This method is used, for example, for thromboses in the abdomen or sinus-cavernosus thrombosis in the head.
In rare forms of vascular occlusions, such as thrombosis in the eye, a specialist ophthalmologist can take an image of the retina and thus diagnose congestion.
Blood test
In addition to imaging, a blood test is also important. This involves searching for degradation products of blood clots, the so-called D-dimers. It should be noted that the D-dimer thrombosis test should only be used to exclude a blood clot if there is a high probability of vascular occlusion. A broad screening is not feasible with this blood test.
Pregnancy
If a thrombosis occurs during pregnancy or after a still/miscarriage, additional examinations should be carried out to find the cause. In this way, a similar course can be avoided if necessary in a later pregnancy.
Other special cases
Even in the case of thromboses that have no clearly identifiable cause or occur in untypical vessels, the doctor will also try to find the cause of the clot formation. Some people, for example, suffer from hereditary diseases that can interfere with blood clotting.
Thrombosis: Course of Disease And Prognosis
A thrombosis is a very serious disease and can lead to dangerous complications. These arise
- when a blood clot dissolves and travels to the heart, from where it can enter the lungs (pulmonary embolism)
- if a vein can be blocked by a thrombus and permanently damaged (consequence: postthrombotic syndrome)
Pulmonary embolism is a particularly common and life-threatening complication of thrombosis. In this process, the thrombus (or parts of it) is washed with the blood flow through the venous system to the right ventricle and from there into the pulmonary arteries. If he lays a large artery there, a large part of the lung is no longer supplied with blood.
It can then no longer participate in the gas exchange, which can lead to a life-threatening lack of oxygen. In addition, the right ventricle can be excessively strained by a high flow resistance; right heart failure is also possible due to pulmonary embolism. An embolism is therefore always a medical emergency!
A pulmonary embolism occurs when part of a blood clot breaks loose and enters the lungs via the heart.
Postthrombotic syndrome
Even if the majority of thromboses heal without consequences, one-third of patients suffer from a so-called postthrombotic syndrome. In this process, varicose veins are formed due to a blood outflow disorder, which remains even after the affected vessels have been reopened. This obstruction of the outflow can lead to further tissue damage or the formation of new blood clots.
Preventing Thrombosis
The best thrombosis prophylaxis (= prevention) is to avoid or reduce the thrombosis risk factors mentioned above. For example, you should make sure you get enough exercise, especially on long flights, but also during long office working days. In addition, a sufficient fluid intake (drinking, liquid food) is important to keep the blood fluid and thus prevent the formation of a clot.
Syringes
After an injury or operation or other immobilization due to illness, the formation of a clot can be prevented with medication: Daily thrombosis injections with heparin can prevent the formation of a blood clot in most cases.
Anti-thrombosis stockings
So-called anti-thrombosis stockings are special elastic stockings made of a skin-friendly, thin fabric, which either reach to the knee or even beyond the knee to the thigh. Due to the slight pressure, they exert on the veins, the blood flows back to the heart somewhat faster and more evenly.
Especially if there are thrombosis risk factors such as a tendency to varicose veins, before and after operations, or for long journeys, wearing anti-thrombosis stockings is recommended. They can often help to prevent thrombosis.