Whooping cough: symptoms, infection, treatment
Whooping cough: symptoms, infection, treatment
Whooping cough (pertussis) is an acute infection of the upper airways. Typical symptoms are convulsive coughing fits and a wheezing sound of breathing during the subsequent air intake. Whooping cough can affect children and adults alike, but it manifests itself somewhat differently. Read here how contagious whooping cough is, how it is treated and why it often remains undetected, especially in adults.

Brief description: Whooping cough
- What exactly is whooping cough? A very contagious, bacterial infection of the upper respiratory tract.
- Symptoms: barking, staccato cough with wheezing after the attacks
- Infection: via droplet infection when sneezing, coughing, speaking or kissing
- Treatment: antibiotics, inhalation, sufficient drinking, spare; patients at risk such as infants should be treated in hospital.
- Vaccination: from the second month of life; must be replenished after ten years and no later than 20 years
- Prognosis: Pertussis can last for several weeks or months, but usually heals completely. Dangerous complications are possible, especially with small children.
Whooping cough – Symptoms
Whooping cough (medically known as pertussis) typically develops in three phases in children:
If you are infected, it is very likely that you will not notice whooping cough at first. In the so-called cold-like phase the symptoms are still unspecific and resemble – hence the name – those of a cold. Only later do typical whooping cough symptoms appear. Classically, a pertussis infection has three stages, each accompanied by different symptoms.
1. Cold phase (stage catarrhale): It lasts one to two weeks. In this first stage the pertussis symptoms are still unspecific. They are therefore rarely interpreted correctly. Usually the complaints are mistaken for a common cold. Whooping cough symptoms of the first stage are:
- Cough
- Sneezing
- Sore throat
- runny nose
2. Attack stage (stage convulsivum): This stage lasts up to six weeks. The classic signs of whooping cough are shown here: spasmodic coughing fits up to shortness of breath (this is why the vernacular also speaks of “stick cough”). The coughing attacks occur mainly at night. After a seizure, patients breathe in with a whooping sound. It is caused by a cramping of the larynx.
A coughing attack often lasts for minutes and can be repeated up to 50 times a day. It occurs in a staccato manner and is therefore also called staccato cough. It is often accompanied by vomiting. At the very least, however, many patients choke out viscous mucus (sputum).
In this stage of the disease, most patients also have no appetite and can hardly or not at all sleep. Fever, on the other hand, occurs only rarely.
3. Recovery stage (stage decrementi): This last stage of the disease lasts up to ten weeks. During this time the coughing attacks gradually become weaker and patients soon feel fitter again.
Whooping cough lasts much longer than a banal dry cough – colloquially it is also called 100-day cough. The type of cough does not differ at first. Only after about three weeks does the second stage of whooping cough occur. Then spasmodic coughing attacks with often panting “gasping for air” after the coughing attack are typical. This stage takes about six weeks. The disease then subsides in the third stage.
In the early stages of the disease, the infection is treated with antibiotics. This prevents complications and also prevents others from getting infected. If whooping cough is discovered too late, only the symptoms are treated. Drink a lot, like bronchial tea. Juicy fruit can soothe after a seizure. Eat light meals if you suffer from gag reflexes. And create cool and humid room air. Also important: rest and physical protection.
Yes, you can still fall ill, but this is much less likely to happen. If adults or children come into contact with the pathogens without vaccination, 80 percent of them fall ill. Whooping cough is therefore very contagious – and especially dangerous for babies. Emergency treatment may be necessary to prevent respiratory arrest. So: Get vaccinated!
Whooping cough in baby and toddler
The younger a child, the more dangerous is whooping cough. In the first year of life, children have not yet built up complete vaccination protection. That is why whooping cough is often severe at this age. In addition, babies and toddlers cannot sit up to cough better.
Another difficulty: Infants often do not show typical symptoms. Whooping cough attacks are often not very strong and not staccato. Often you only notice a beep or a little reddened face. The focus is often on breathing stops (apneas): the little ones stop breathing for seconds. The skin may become partially bluish (cyanosis) due to the difficulty in breathing.
Other possible complications include pneumonia, otitis media and encephalitis with seizures). Unvaccinated infants under six months of age, premature babies and babies of very young mothers are particularly susceptible to severe whooping cough disease.
Whooping cough: symptoms of concomitant diseases
The typical symptoms of whooping cough can be accompanied by other symptoms when patients develop a concomitant disease. This happens in about a quarter of all patients. The reason is usually that whooping cough is diagnosed and treated late. The bacteria have then often already spread in the body. Possible concomitant diseases and subsequent symptoms of whooping cough are
- Otitis media and pneumonia: These occur when the pertussis bacteria migrate up the auditory canal or down into the lung tissue.
- Hernia of the ribs and inguinal hernia: These are caused by particularly severe coughing attacks. Often these fractures are only detected much later, for example when severe pain occurs during sports.
- severe weight loss: This is particularly common in children. Pertussis is often accompanied by a lack of appetite.
- Incontinence: It is primarily a problem of children and elderly people. With every coughing attack, a large pressure is built up in the body. Then some urine can be released uncontrollably. But incontinence is not a permanent problem. It disappears again as soon as the pertussis symptoms subside.
Pertussis: risk of infection and incubation period
Whooping cough is contagious, even very contagious! Without vaccination, 80 to 90 percent of people who come into contact with the pertussis pathogen fall ill. Whooping cough is transmitted via droplet infection: when infected persons speak, cough or sneeze, tiny droplets of saliva are distributed in the surrounding area – within a radius of up to one meter. These small droplets contain pertussis bacteria. If they reach the mucous membrane of a healthy person (for example, by inhalation), this person will also be infected.
Pertussis infection is also possible through kisses. This also applies if you use the same cutlery as a sick person.
Even if you are vaccinated against whooping cough and do not become ill yourself, you can still become a carrier of the bacteria for a short time. In this way you can pass the germs on to other people unnoticed.
Bordetella pertussis: The bacterium Bordetella pertussis causes whooping cough.
Whooping cough: Incubation period
As with most infectious diseases, pertussis can take some time to show the first symptoms after infection. This so-called incubation period is about seven to 20 days for pertussis. Those affected are contagious from the onset of the first symptoms (cold phase) and then for another five to six weeks. Exception: treatment with antibiotics shortens the infection phase. Thus, five days after the start of therapy, a patient is no longer contagious.
The best way to protect yourself from whooping cough is to avoid contact with sick people. In case of illnesses in the family you should pay attention to careful hygiene.
Whooping cough in adults
Whooping cough was long considered a “childhood disease”. But he’s not anymore. Increasingly, young people and adults are also falling ill with it:
In 2008, the average age of pertussis patients was about 42 years. Ten years earlier, it was still about 15 years. Meanwhile two thirds of all whooping cough cases affect people older than 19 years! According to medical experts, this is due to the fact that adults often forget the necessary booster vaccination: Almost all children (95 percent) are vaccinated against pertussis when they start school. However, this vaccination protection must be refreshed after ten to a maximum of 20 years. Those who do not do so will catch whooping cough at the next opportunity and most likely become ill.
Whooping cough in adults often takes an untypical course: The symptoms are weaker, the coughing attacks less severe and more continuous than attacks. The risk of suffocation is low.
However, this does not make the infection any less dangerous; on the contrary: many ill adults simply consider whooping cough to be a particularly persistent but common cough. You don’t go to the doctor for this. However, without treatment the whooping cough pathogens can spread throughout the body. In rare cases this leads to complications and secondary diseases. Often, for example, pneumonia or middle ear inflammation as well as broken ribs are the result of whooping cough.
Adults who suffer from pertussis are also often a danger to others. They are considered a serious source of infection for infants and the elderly. With these, whooping cough can be severe and dangerous.
Pertussis & Pregnancy
Pertussis during pregnancy does not endanger the child. However, violent coughing attacks can trigger premature labour. The infection also weakens the expectant mother.
Women who want to have children should therefore be vaccinated against whooping cough up to three months before pregnancy. If this is no longer possible, a pertussis vaccination should be given in the first days after birth. It also means a certain protection for the baby if the mother cannot get whooping cough.
Pregnant women who have not been vaccinated should avoid any contact with those who are ill. If you suspect an infection, your doctor may prescribe an antibiotic (erythromycin) as a precautionary measure. This alleviates the symptoms of whooping cough.
It is very unlikely that whooping cough bacteria are transmitted from an infected pregnant woman to the unborn child.
Whooping cough: causes and risk factors
The cause of whooping cough is the bacterium Bordetella pertussis. It attacks the nose, throat, windpipe and lungs and irritates the mucous membranes. This triggers the convulsive coughing fits.
The bacterium also secretes various toxins. On the one hand, these damage the surrounding tissue (especially the cilia of the mucous membranes in the airways). On the other hand they weaken the immune system. As a result, the body can no longer defend itself sufficiently against the bacteria. The germs can thus reproduce undisturbed. Untreated whooping cough can therefore cause serious complications and even be fatal.
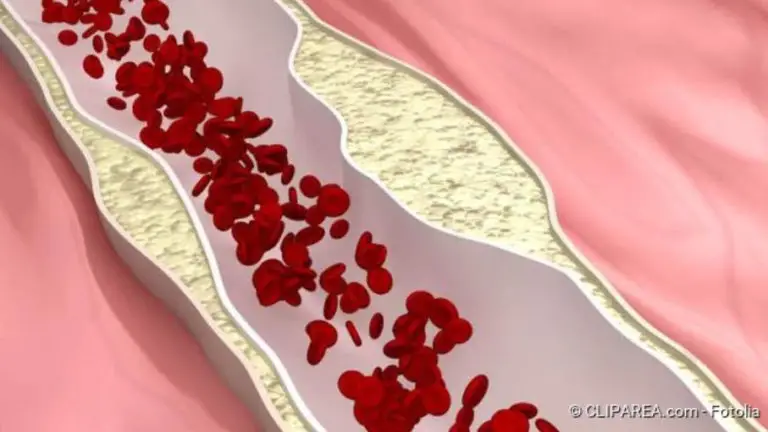
Infection and course of disease: In whooping cough, bacteria enter the upper respiratory tract via microdroplets. They destroy the mucous membrane and thus trigger spasmodic cough attacks.
In addition to Bordetella pertussis, related species can very rarely cause a whooping cough-like disease. These are Bordetella parapertussis and Bordetella holmesii. In most cases, however, an infection with these pathogens is shorter and less severe.
Whooping cough: examinations and diagnosis
To clarify the suspicion of whooping cough, the doctor will first take the patient’s medical history (anamnesis). To this end, he talks to the patient or – in the case of small children – to the parents about the complaints that occur. Typical questions here are:
- How long has this cough been going on?
- Is coughing up mucus or is the cough rather dry?
- Do you have problems catching air after coughing attacks?
- Are there any other complaints (fever, sore throat, chest pain etc.)?
The doctor will also examine the patient physically. This includes tapping the chest and listening to the lungs. He also takes a look down the throat. If it presses the tongue with the spatula, it triggers the characteristic coughing attacks in whooping cough.
If the typical pertussis symptoms (in children) are present, this makes the diagnosis easier. Laboratory tests should be performed for confirmation (see below).
Such laboratory tests are even more important if whooping cough is untypical. This is mainly the case with babies, but also with adolescents and adults. The latter now represent the most frequent age group among pertussis patients.
Laboratory tests
The type of laboratory tests used depends on the stage of the disease.
In the first two to three weeks after the start of coughing, an attempt is made to detect the whooping cough pathogen directly. To do this, the doctor either takes a smear from the deep throat or sucks out some bronchial mucus, which is transported upwards when coughing.
In the laboratory, the sample can be placed on a culture medium to grow the germs (bacteria culture) and then determined. Alternatively, the genetic material of germs contained in the sample can be amplified by means of polymerase chain reaction (PCR) and then identified. This is another way to detect the pertussis pathogen – if present.
Another possibility besides the direct detection of the pathogen is the so-called serum diagnostics. The patient’s blood serum is tested for antibodies against the pertussis pathogens. However, this method is only possible in advanced stages of the disease: Such specific antibodies are only detectable about three weeks after the onset of coughing.
If the doctor suspects complications or secondary diseases of whooping cough (such as inflammation of the middle ear or pneumonia), further examinations are necessary.
Whooping cough is notifiable
Since the year 2013, there is an obligation to report whooping cough in the European Union: If pertussis is suspected and the disease is proven, the doctor must disclose the name of the patient to the responsible health authority. Death by pertussis must also be reported.
Whooping cough: treatment
As with other diseases, the following applies to pertussis: therapy and healing process depend on the stage and severity of the disease.
Pertussis therapy for children
Whooping cough in children can usually be treated at home if the disease is mild. In severe cases, treatment in hospital is advisable. The same applies if a child has previous heart or lung diseases.
Infants with pertussis should always be treated as inpatients. In the clinic the bronchial mucus can be sucked out – babies are not able to cough up the mucus. In addition, quick and professional action can be taken if breathing stops threaten or occur.
Sick children should generally receive a lot of attention and affection. Strict bed rest is not necessary with whooping cough. It is enough to take it easy on the body. Walks in the fresh air and quiet play are allowed and may even be good for you. However, make sure that the environment is low in irritants.
Calm the child down if he has a coughing attack. It can also be helpful to put it on or carry it around. Inhalation over a bowl of hot water and sea salt can relieve the symptoms in older children. For small children, the pharmacy has inhalation devices with which they cannot scald themselves.
Warm chest compresses with lemon juice before going to bed can also alleviate the pertussis symptoms a little.
The room air should not be too dry. For example, you can air the room regularly or hang damp cloths over the heating. This increases the air humidity.
The patients should drink enough. Preferably prepare liquid or mushy food. Several small meals spread over the day are more advisable than a few large meals. Children with whooping cough tend to gag and vomit.
Make sure that your child does not come into contact with other children or older people during the infection period. These are particularly susceptible to infection and possible serious courses and complications.
Antibiotics can reduce the duration and severity of coughing attacks in whooping cough. However, this only works if they are administered as early as possible, i.e.: before or in the first one or two weeks after coughing.
Under certain circumstances, however, antibiotic treatment may still be useful afterwards: The symptoms can then hardly be influenced. However, antibiotics can be used to break the chain of infection: Approximately five days after the start of intake, patients are no longer infectious. They are then allowed to visit community facilities such as schools and kindergartens again.
Antibiotics used include erythromycin and clarithromycin. They are taken for a few days to two weeks depending on the active ingredient.
Cough syrup usually helps little or not at all with pertussis. If the mucus formed in the bronchi is very viscous, sometimes expectorant drugs can help.
Pertussis therapy for adults
Whooping cough in adults is treated similarly to that in children. Antibiotics are preferably given in early stages of the disease. In later stages they serve to reduce the risk of infection for other people. This is particularly important for adolescent and adult patients. Often it is they who infect babies. And for these, whooping cough can be life-threatening.
Besides antibiotics, general measures support the treatment of whooping cough. These include inhalations, chest wraps, an adequate fluid intake and humidified room air.
Employees of community facilities (such as teachers, educators, nursing staff, etc.) may not go back to work until the attending physician allows them to do so. Only he can judge whether the patient can still transmit whooping cough pathogens to others or not.
Whooping cough vaccination
You can protect yourself from whooping cough with a vaccination. The whooping cough vaccination is recommended in early childhood. It can be administered from the second month of life. Regular booster vaccinations maintain the protection against whooping cough, even in adulthood. Especially the following groups of persons should be vaccinated against whooping cough:
- Women of childbearing age
- close contact persons of pregnant women in the same household and caregivers (e.g. childminders, parents, siblings) if possible four weeks before the birth of the child
- caring parents of a child with pertussis
- Employees in the health service and community facilities
You can read more about this in the article whooping cough – vaccination.
Whooping cough: course and prognosis
Whooping cough can last for weeks to months. In some patients the disease is relatively mild, in others it is severe. However, pertussis usually heals completely without permanent damage.
However, about one in four whooping cough patients develop complications. These include, above all, pneumonia and inflammation of the middle ear. Children are affected more often than adults.
Especially for babies under six months whooping cough can be very dangerous. The breathing stops can cause a considerable lack of oxygen, which damages the brain. Possible consequences are permanent damage such as paralysis, visual or hearing disorders and mental disorders. Very rarely the little patients even die. Therefore, as a precaution, infants with whooping cough should always be treated in hospital.