Nuchal Cord And Fetal Death: Complate Investigation
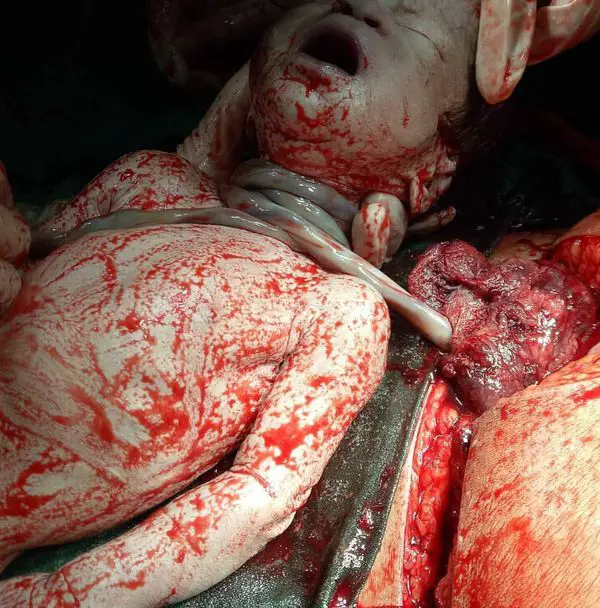
Nuchal Cord
Nuchal cord is a risky situation that occurs during the pregnancy, a condition that may affect the labor and may complicate the delivery of the child. It is a condition that happens in the cases that the cord, the umbilical cord of the baby, is wrapping his neck. If it gets too tight in wrapping the neck, it may reduce the blood flow through the veins, which means that a child would not get enough of oxygen and other vital nutrients and thus affect child’s growth. Further, as one can imagine that giving birth to a child with the umbilical cord encompassing the neck similar to a rope is not an easy task and there is a risk of severe asphyxia and damage to the brain (cerebral palsy).
In human beings or placental mammals, umbilical cord is a narrow cord of tissue that connects the fetus to the placenta lying in the maternal womb. During pregnancy, umbilical cord develops from the remnants of yolk sac and allantois by the fifth week of fetal development. On average, umbilical cord is 55 cm long with diameter of 1-2 cm. It works as a conduit or passage between fetus and placenta, comprising of two arteries and a vein. It supplies oxygen and provides nutrients to the developing baby and eliminates waste products from the baby. Various complications of the umbilical cord have been studied ranging from false knots to lethal vasa previa. False knots have no clinical significance while vasa previa often ends up with fetal death. Other umbilical cord abnormalities include single umbilical artery, umbilical cord prolapsed, nuchal cord, umbilical cord strictures and cysts. In this article, we will only elaborate nuchal cord and its clinical significance.
Nuchal cord refers an abnormal condition when umbilical cord loops around the fetal neck for 360 degrees. Nuchal cord is called single, double or triple nuchal cord depending upon the number of umbilical cord loops wrapped around the neck for ≥360 degrees. History of nuchal cord dates back to 1962 when J. Selwyn Crawford defined it as “360 degrees around the fetal neck.” The incidence of nuchal cord varies with gestational age and associated risk factors. On average, its incidence is 10-29%, which increases with advancing gestation age. There are no specific signs and symptoms of nuchal cord. However, if the baby begins moving less at 37 weeks of gestation, it may be a possible alarming sign of nuchal cord. Additionally, monitoring during labor can identify bradycardia.
As the child grows in a mother’s womb, it is surrounded by amniotic fluid and is fed by mother through an umbilical cord. The umbilical cord is responsible for bringing both the nutrients and oxygen to the growing organism. This umbilical cord is attached to the wall of mother’s uterus with the help of root-like structure called placenta on one side, and to child’s navel on another side. Therefore, the umbilical cord is the main artery, vein, and a lifeline of a child. If anything goes wrong with it, a child may suffer. Though fortunately, complications related to the umbilical cord are uncommon, and even if they occur they often resolve spontaneously without any medical intervention. Nature has its own ways to resolve the problems. Though sometimes trouble with an umbilical cord may arise.
Umbilical cord is quite thick with an average diameter of around 3 cm (centimeters ad meters are used to measure umbilical cords). It is also lengthy too, and in most cases, it is about half a meter. Though there are lots of individual variances, thus umbilical cord maybe anything between 20-30 centimeters to even three meters. Yes, in few cases it can get pretty long. After about three months of pregnancy, a child becomes quite an active and starts making lots of movements in the womb. So as one can guess that there is a risk of the umbilical cord getting tangled around a child, after all, it looks like a rope, roughly speaking.
What is the Situation Known As Nuchal Cord?
There is no fixed data on the nuchal cord, the reason perhaps behind this, is that it goes unnoticed in a large number of cases, and moreover the cord position keeps changing during the course of pregnancy. However, experts estimate that it is present in about 10-30% of cases. Right, that number is quite significant, but as we already mentioned, in the vast majority of cases the problem would resolve spontaneously without any medical intervention. in a few cases, this condition may get worse and the umbilical cord may even further tighten around the neck.
In modern times, the nuchal cord can be diagnosed in the majority of the cases through the regular use of ultrasounds. Although earlier ultrasounds were not good enough, however, latest color Doppler’s can detect nuchal cord in more than 80% of cases. Once it has been diagnosed, medical specialists have to make preparations accordingly, in some cases, they may go for cesarean section (C-section) instead of natural birth. In these cases, C-section has to be performed quickly and with particular skills so that to avoid making ischemia worse. Further, after the birth, there is often the need for extra care in a child with a nuchal cord antecedent.
It is natural to ask if the nuchal cord can kill a baby by strangling? Yes, such risk is always there. Though in the vast majority of cases this situation improves with the progress of pregnancy, however, in a small number of instances it may become worse. In some cases, the umbilical cord may get very tightly wrapped around the neck of the baby thus causing asphyxia. In few cases it may hinder the baby’s growth, in worst few cases it may even lead to baby’s death, though such outcomes are not common. Further, in the nuchal cord, there is a risk that a child may get strangled during the birth process when the umbilical cord is pulled.
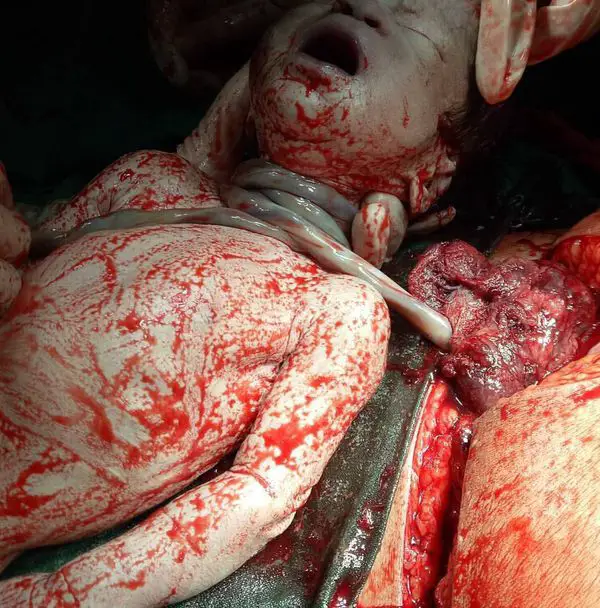
There are two types of nuchal cord: Type-A and Type-B. Type-A nuchal cord freely encircles the fetal neck in a sliding pattern while Type-B nuchal cord wraps around the neck in a locked pattern. Type-A nuchal cord can undo itself spontaneously while type-B nuchal cord cannot undo itself spontaneously. Remember, nuchal cord unlikely develops or corrects itself during labor. If nuchal cord is tightly wrapped around the neck, it may result in catastrophic outcome, presenting as strangulation of the fetus, which can be identified with presence of features such as dusky face, facial bruises, hyoid bone fracture, facial suffusion and conjunctival hemorrhage. Additionally, vagal collapse may occur due to compression of carotid sinuses by the tight loop of umbilical cord. In nuchal cord strangulation, umbilical cord itself works as a noose; hence subjects the developing baby to collapse, as it is the only source of oxygen and nutrition to the fetus. Grading of tight nuchal cord is given as:
- If conjunctival hemorrhage and petechiae or bruises are present at the time of delivery, it is thought to be due to grade-1 nuchal cord
- If the delivered baby is having dusky face, facial suffusion along with pallor, it indicates grade-2 nuchal cord.
- If respiratory distress, stupor and decreased body tone are identified at the time of delivery, it is the result of grade-3 nuchal cord.
Unexplained stillbirths are usually attributed to compromised umbilical circulation. Clinical assessment along with the presence of vascular ectasia and thrombosis within the umbilical circulatory system indicates cord accident.
Ultrasonography, especially Doppler scan, is considered the gold standard non-invasive investigation for the detection of nuchal cord, usually after 36 weeks of pregnancy. Multiple views of fetal neck are looked for nuchal loops. If an umbilical loop encircles up to three-quarters of the neck, it is termed as nuchal cord. Another clinical test involves transabdominal manual compression of fetal neck. In this test, if the baby develops bradycardia, the test is positive. It indicates cord compression and requires close monitoring of the fetus.
Various risk factors have been identified which predispose to nuchal cord development during gestation. These risk factors are induction of labor, African-American infant race, primi-parity, male baby, marginal cord insertion, excessive amniotic fluid and fetal movements, twin pregnancy, abnormally long umbilical cord, fetus large for gestational age, nutritional deficiencies, breech presentation and post-term pregnancy. Nuchal cord may develop secondary to a random event.
Nuchal cord is an obstetric challenge in terms of clinical management! It depends upon various factors including number of loops, fetal growth, gestational age, amniotic fluid index (AFI) and others. Close monitoring is needed for multiple nuchal loops wrapping the fetal neck. The obstetrician may plan for early delivery if multiple loops are noticed on Doppler scans. Successful management of nuchal cord is avoiding early clamping or cutting of the cord and discouragement of unnecessary interventions. The Somersault manoeuvre is often encouraged if tight nuchal limits the descent of baby.
Nuchal Cord and Birth Asphyxia
One of the reasons why this matter is so difficult to predict is the considerable variance in length and circumference of the umbilical cord. Moreover, this situation evolves notoriously during the pregnancy. In most cases, as already mentioned, the umbilical cord is about half a meter. It has two arteries for supplying nutrients to a child and a vein to take back the deoxygenated blood. In some cases, the umbilical cord may have just one artery. Nuchal cords are of two types, classified according to the severity:
Type A nuchal cord is when the umbilical cord is wrapped around the baby’s neck 360 degrees. Type B nuchal cord is more severe form when the cord is wrapped in a manner that it cannot be undone.
Nuchal cord is an immensely common phenomenon; it may form and resolve more than once in a single pregnancy. Thus, nuchal cord may develop, a child may get tangled, and then after a few weeks may again become detangled. In the majority of cases problem would resolve, and in some circumstances, it would persist. Simply stated, it is difficult to predict and to observe. Effects of nuchal cord on fetal development are varied. In some cases, it may not harm at all, while in other cases it may reduce the supply of nutrients and thus preventing the proper fetal development. In some cases, it may affect the delivery process while in others it may not have any effect. Some of the ways by which nuchal cord may harm the child/fetus and lead to complications are:
- The umbilical cord may get tightly tangled around the neck and thus restrict the blood blow to the brain through the vital fetal artery called carotid artery.
- It may cause congestion of backflow of venous blood of umbilical cord.
- Compression of umbilical cord arteries.
Nuchal Cord Complications and Birth Injuries
Though the majority of cases of nuchal cord would not have any adverse outcomes, and it would not harm a child during the birth process, nevertheless, in some cases, it may cause severe development issues and may also lead to birth injuries. or even death.
How dangerous is nuchal cord would depend on the number of factors like how tight is the cord around the neck. Is the nuchal cord wrapped around the neck just once or more than once? Other conditions in the womb like the amount of amniotic fluid would also influence the severity of the condition.
Following are the common complications of nuchal cord, especially of the so-called tight nuchal cord:
- Birth asphyxia or Hypoxic-ischemic encephalopathy (HIE)- is the most common of all the injuries, it is a condition when the child’s brain does not receive enough of oxygen and nutrients especially during the near term, and thus resulting in various developmental complications. Such a child may have developmental disabilities, cerebral palsy, and learning disabilities.
- Fetal death- although rare, but happens in some cases when the nuchal cord is too tight, thus resulting is strangling of the baby.
- Intrauterine growth restriction- again it is more common in the tight wrapping cord, which is present in a small number of cases. In such instances, the baby does not receive enough of oxygen and other nutrients. Sometimes a doctor may decide to do C-section before term to avoid any further complications.
- Higher risk of meconium aspiration syndrome- since in tight nuchal cord a child is almost strangled and is struggling to breathe, thus it may cause a child to start breathing in meconium, which is a mixture of fecal matters and amniotic fluid. If this contaminated mixture enters the child’s lungs, it may lead to various complications.
- Various cardiac and metabolic abnormalities- since the lack of nutrient forces the heart to beat faster and body to make multiple adjustments, such a child is at higher risk of developing various complications after the birth. How nuchal cord affects the health of survivors is still a matter of research.
- Neurodevelopmental abnormalities are perhaps worse of all since in such conditions child survives but fail to thrive.
Causes and Risks of Nuchal Cord
Nuchal cord is poorly understood phenomenon since only high-resolution color Doppler’s have made its study possible. Nonetheless, the risk of nuchal cord and its complications can be predicted to some extent. Specific cases are at higher risk:
- A fetus which moves too much is at higher risk of becoming tangled.
- Risk also depends on the length of umbilical cord, greater the length, higher the risk.
- In the majority of cases, it is just a random event.
Considering the various risks involved, one may ask that at what point of pregnancy a woman may learn about the nuchal cord? Research indicates that risk increases with the gestational age, thus at 20-week nuchal cord is present in less than 5% of cases while at 42 weeks it may be seen in one-third of cases. It should be noted that monoamniotic twins that are twins that share the same amniotic sac are at much higher risk of nuchal cord, as per some estimates it is present in almost all the cases.
Factors that increase the risk of the nuchal cord are:
- Unusually long umbilical cord
- Multiple gestational pregnancies like twins or triplets
- Too much of amniotic fluid and thus extra space in the womb (means higher fetal movement and risk of getting tangled)
- An abnormal fetal position like shoulder presentation
- Baby too large for gestational age
How Is Nuchal Cord Diagnosed?
Ultrasound is the gold standard as it is safe and technology is improving too. Moreover, pregnant women would go through ultrasound for more than once for various reasons. In ultrasound, the physician would pay particular attention to the location or position of the umbilical cord, and nuchal cord would be diagnosed if it is seen encircling three-quarter of the neck. If a physician sees that umbilical cord only encircles half of the neck than the situation would be called suspicious, it means that there is a need for further investigations. It must be understood that at present there is no 100% sensitive method of nuchal cord detection. Moreover, diagnoses may be missed if nuchal cord happens late in the pregnancy. At present, the chances of nuchal cord detection in grayscale ultrasound are not more than 70%, though color Doppler’s are much more effective and may detect nuchal cord in 80-90% of situations.
Diagnosis of a nuchal cord is difficult without the ultrasound, but it may be expected if a to be mother notices that there has been a sudden decrease in the fetal movement after the 37 weeks or if a doctor detects abnormal fetal heart rate.
Treatment of Nuchal Cord
There are few things to understand; nuchal cord is not an indication for C-section until or unless ultrasound shows that it is a tight cord, or the umbilical cord is wrapped several times around the neck of the fetus, and thus there is high risk in natural birth.
In most cases, things are either mild or would resolve by themselves. In those small number of instances where nuchal cord persists, doctors know the specialized techniques of childbirth to prevent complications. Like they slip the cord over the infant’s shoulder during the delivery process, or in rare cases, they may go for early clamping of the cord. In these situations however, cord blood banking will not be possible, the cord blood cannot be generally collected with the aid of the collection kit and cannot be stored in a public or private cord blood bank to separate the valuable baby stem cells and bank them afterwards.
In short, if the nuchal cord has been diagnosed, It is better to give birth in the decent clinic under the supervision of trained specialists, which would minimize the risk.
In few cases, a child may receive some minor trauma due to tangling of cord. Most modern clinics are well prepared to handle such complications, and the majority of infants would recover quickly and completely from such injury. Facial duskiness and facial petechiae may be caused in some cases.
In conclusion, it can be said that nuchal cord does increase specific risks. Nonetheless, most current medical teams are well trained to handle these complications and thus prevent any long-term harm to the child’s health. Though minimal risk exists, considering that the childbirth is a complicated process and nothing less than a miracle.