Brown spots on skin: Are they dangerous?
Brown spots on skin: Are they dangerous?
Brown spots on the skin (also called pigmentation or hyperpigmentation) can appear in many forms, for example as age spots, birthmarks or freckles. Some types occur only sporadically, others occur over a large area and on the whole body. Most species are completely harmless – but every now and then there can be more serious diseases behind it. Here you can find out what types of stains there are, how brown skin discolouration develops and when it makes sense to consult a doctor.
Causes
What types of brown stains are there?
Brown spots on the skin come in many different forms – and depending on the cause, they can vary considerably. In the following we present the most important types of brown stains.
Moles and birthmarks on the body
The pinhead to pea-sized moles or liver spots are brownish accumulations of pigment rich cells. These can be so-called melanocytes, which normally release their pigment, melanin, to the skin and thus ensure that the skin turns brown. The medical term for moles is short nevus. These are often congenital. The risk of developing skin cancer from these small patches is slightly increased. Therefore, regular check-ups by the dermatologist are absolutely recommended. Read about what to look out for in moles.

Age spots on face and hands


Melasma, Chloasma, pregnancy mask
These are yellowish-brown skin discolorations, which occur mainly in women during and after pregnancy. The extensive hyperpigmentations occur especially on the cheeks, around the mouth, on the forehead and on the temples. The triggers are primarily hormonal changes – for example during pregnancy, when hormonal contraceptives are inserted or discontinued or when hormone replacement products are used. Read more about causes and treatment of melasma.
Melanomas (skin cancer)

In addition to the types of skin discoloration mentioned above, there is a whole range of other forms with very different characteristics:
-
Cheeky dots: freckles
-
Everyone knows the small light to dark brown, often also reddish-brown spots. They appear mainly on the face, neck, shoulders, arms and hands – the very places that are more often exposed to the sun. The predisposition is hereditary and they are caused by a gene variant. Freckles are neither dangerous nor harmful, but are mainly found in people with fairly light skin colour, who are more sensitive to the sun. Read more about how freckles develop and what can be done about them.
-

Freckles occur mainly in people of Nordic origin, who generally have very sun-sensitive skin. -
Café-au-Lait-Spots
-
As the name suggests, these even and not raised stains are reminiscent of coffee with milk. They can be of different sizes and are clearly distinguishable from their surroundings. Mostly they appear on the trunk and the limbs. These are congenital spots, which often appear in infancy and childhood. They are usually harmless, but can be a sign of neurofibromatosis (Recklinghausen disease), among other things. 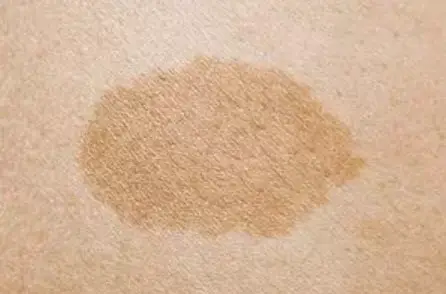
Six milky coffee stains are considered to be the limit value. Those who have more of these hyperpigmentations should have them examined, as they can indicate various diseases. -
Spots after inflammatory skin diseases
-
So-called post-inflammatory hyperpigmentations may occur after a skin inflammation has healed – typically after acne inflammation, neurodermatitis or psoriasis, but also after wound healing (e.g. by dermabrasion, chemical peeling or laser treatment). Here you can learn more about post-inflammatory hyperpigmentation.
-

During post-inflammatory hyperpigmentation flat discolorations are formed. -
Bacterial infection: Erythrasma
-
This is a superficial bacterial infection of the skin. Triggers are corynebacteria, which are naturally present on the skin. In places where skin rubs against skin (e.g. under the armpits, in the groin area or under the breasts) these bacteria can multiply and penetrate the uppermost layer of skin. This usually results in slightly scaly skin redness, which usually does not cause any complaints. This infection is favoured by increased sweating, overweight, diabetes and immunodeficiency diseases. 
Erythrasma is also known in German as dwarf lichen. -
Skin spots due to medication
-
There is a whole range of different medications that – especially in combination with UV light – can lead to brown spots on the skin. These include
- topical (i.e. locally applied) medicines, e.g. for acne
- Antimalarial drugs like chloroquine
- Chemotherapeutic agents for cancer treatment sometimes cause skin discoloration over veins or on nails.
- hormonal contraceptives (see above under “Melasma”)
- certain agents against cardiac arrhythmia and rheumatism
- some drugs for psychoses (neuroleptics),
- various antibiotics and medicines containing St. John’s wort extracts.
Thus, those who have light skin that is prone to sunburn should therefore not go out in the sun for too long and under no circumstances go into the sun without adequate sun protection or go to a solarium as long as an appropriate medication is taken.

There is a whole range of different drugs and medicines that can cause brown spots on the skin. -
Stains after phototoxic reactions
-
Phototoxic dermatitis can also lead to permanent discoloration of the skin. It can be triggered by various substances such as:
- Perfumes and skin care products, especially with bergamot oil and tea tree oil
- certain plants (giant hogweed, daisy family, lily family and others)
- Metals and other chemical substances (e.g. in pharmaceuticals)

Tea tree oil is considered by many to be a remedy for eczema or pimples – but its use can lead to skin discoloration. -
Stains due to venous insufficiency
-
With venous insufficiency, the blood circulation in the legs is disturbed. The pressure in the veins increases and fluid gets into the surrounding tissue and the skin is less nourished. As a result, blood cells get into the skin tissue, decay there and the iron from the blood pigment leads to visible brown spots on the skin. Since melanin does not play a role in this form of hyperpigmentation, but rather deposited iron, the color of the spots is less brown, but rather red-brown to bluish. 
Chronic venous insufficiency is usually accompanied by spider veins, varicose veins and swollen legs that are sensitive to touch and pain. -
Purpura pigmentosa progressiva (Purpura stains):
-
Purpura pigmentosa progressiva (also known as Schamberg’s disease) is a chronic, intermittent skin disease in which the smallest vessels (capillaries) become inflamed. The cause is not clear. Possible triggers are drugs and trigger factors are food, food additives and contact allergens, e.g. in textiles. The disease causes skin bleeding that starts on the lower legs. Typical are irregular brown-red skin spots of different sizes with surrounding, partly reddish spots, comparable to peppercorns (“cayenne pepper spots”).
-
Brown spots in metabolic and systemic diseases
-
Iron storage disease (hemochromatosis) is an inherited liver disease in which the body is no longer able to properly store or break down absorbed iron. It accumulates in the tissues of many organs, including the skin.
Also inherited is the protein metabolic disease alkaptonuria. Brownish to bluish-black discoloration of the skin, often on the ear, eyelids, nose, cheeks and hands, is typical.
Brown spots that form around scars can occur in connection with the systemic disease sarcoidosis.
Peutz-Jeghers syndrome is a hereditary disease that leads to intestinal and gastric polyps and tumours of internal organs. At first, brown, liver spots around the mouth, on lips, mouth mucosa and back of the hand are conspicuous.
Causes and backgrounds
How do brown skin spots develop?
As shown above, brown patches on the skin can take many different forms: from small and sharply defined to large and frayed. They appear individually or in groups, some are a little raised, but most are completely smooth. These brown discolorations can occur basically anywhere on the body. They can be congenital or develop only in the course of life
Responsible for such brown discolorations on the skin is usually a local overproduction of the pigment melanin (or a local increase in melanocytes), which gives our skin, hair and eyes the actual color. Other causes can be:
- smallest bleedings in the legs due to vein weakness
- Metabolic disorders e.g. due to liver disease
- Systemic diseases or hereditary diseases
- Contact with chemical substances such as silver salts or phenols


In addition, there are various factors that can promote an overproduction of melanin: The most important are sunlight, genetic predisposition, metabolism, hormonal influences, ageing processes and skin injuries. Certain drugs may also play a role.
Active cancer prevention: Check brown spots: When should I see a doctor?

-
The ABCDE rule for birthmark check
-
- A (Asymmetry)A spot is conspicuous if its shape is not uniformly round or oval.
- B (Limitation)A pigment mark should be sharp and regularly limited. A blurred, washed-out border and irregular fraying or runners on a pigment mark are grounds for caution.
- C (Colour)Birthmarks with several shades of colour should be checked.
- D (Diameter)A pigment mark whose diameter is greater than 5 millimetres should always be observed.
- E (prominence + development)Pre-curved and palpable moles should also be checked – as well as moles that change shape or colour.
Here you can learn more about how to recognize suspicious pigmentation marks.

![]()
If you observe new discolourations on the skin, these will be completely harmless in most cases. In order to rule out that these are the signs of illness, a medical examination should be carried out. Possible concomitant complaints such as fatigue, fever or joint pain may, but do not have to be related to this. In any case, a visit to the doctor will provide clarity and, if necessary, enable the introduction of appropriate medical measures through professional diagnosis.





