Histamine intolerance: symptoms, description, causes, test
Histamine intolerance: symptoms, description, causes, test
In case of histamine intolerance, the body reacts to an increased amount of histamine with intolerance reactions. This substance occurs naturally in the body, but is also found in many foods. Possible symptoms of histamine intolerance are wheals on the skin, itching, headaches and gastrointestinal complaints. Mostly middle-aged women are affected. Read all about histamine intolerance.

Brief overview
- What is histamine intolerance? Incompatibility with large amounts of histamine. Histamine is a tissue hormone and messenger substance that occurs naturally in the body. But it is also found in many foods. However, histamine intolerance (HI, histaminosis) is a controversial clinical picture among experts.
- Symptoms: very varied, e.g. reddened skin with a feeling of heat (flush), itching, hives (urticaria), palpitations, headaches, stuffy or runny nose, asthma, diarrhoea, abdominal pain
- Causes: Experts suspect an acquired or (more rarely) congenital disorder of histamine degradation in the body.
- Investigations: Doctor-patient consultation to take the patient’s medical history (anamnesis), examinations to exclude other possible causes for the complaints, three-stage dietary change, possibly a provocation test
- Treatment: adapted diet, possibly enzyme preparations
Histamine intolerance: symptoms
Symptoms of histamine intolerance are very diverse. Some patients only show individual symptoms (such as reddening of the skin with itching). In others, however, histaminosis manifests itself with symptoms in several parts of the body. This is because the most diverse cells and organs have docking sites (receptors) for histamine. These include smooth muscle cells (in the stomach and intestinal wall, in the bronchi and uterus, in the blood vessel walls etc.), gland cells, nerve cells and cells of the immune system (such as mast cells).
Histamine mediates its effect by binding to these receptors. In case of a high amount of histamine, the receptors are activated continuously. Depending on where in the body they are located, this results in the most varied histamine intolerance symptoms in sensitive people.
Histamine intolerance symptoms: Skin
In the skin histamine can activate so-called mast cells. These then release allergenic ingredients that can cause various skin symptoms:
- Urticaria (hives): It is characterized by small, volatile swellings of the skin (wheals), which are usually beet-like. The skin usually appears red or white with a red border in the affected areas. The wheals can occur all over the body. They usually disappear after 24 hours. However, as long as the trigger of hives persists, new hives can form.
- Itching: The substances released from the mast cells cause urticaria as well as massive itching. Especially the skin above the wheals is very irritated. In contrast to other itchy skin diseases, however, hives are not scratched, but only rubbed and pressed.
Histamine intolerance symptoms of the skin also show up in an increased blood circulation: histamine leads to a release of nitric oxide, which dilates the blood vessels. So more blood can flow through. As a result, the affected skin areas are reddened and warmed. If this phenomenon occurs on the face, it is also called a flush.
Histamine intolerance symptoms: Brain
In the brain, histamine can also cause blood vessels to dilate by releasing nitric oxide. If this happens to the arteries of the meninges, headaches can occur. This mechanism is also discussed for migraine.
Other possible symptoms of histamine intolerance that can emanate from the head are dizziness, nausea and vomiting. Some patients also report reduced attention and fatigue.
Histamine intolerance symptoms: Cardiovascular system
If histamine alters the width of the coronary vessels (coronary arteries), tachycardia and cardiac stuttering (extrasystoles) may occur. These are mostly harmless cardiac arrhythmias. Some patients also report palpitations.
If the blood vessels in the periphery of the body dilate, the blood pressure can drop. In extreme cases (with very high amounts of histamine), the blood in the legs can sink so that not enough is transported back to the heart: This causes the blood pressure to drop sharply and shock symptoms may occur. But that happens very rarely.
Histamine intolerance symptoms: Gastrointestinal tract
In the stomach histamine increases the production of gastric acid. The muscle cells in the wall of the gastrointestinal tract are also more strongly activated by histamine. Therefore, abdominal pain or cramps, diarrhoea and flatulence are common histamine intolerance symptoms in the digestive tract. They occur mainly when consuming histamine-rich foods and beverages.
Histamine intolerance symptoms: Genital tract
In women, histamine is produced in the uterus and ovaries, among other places. It is said to increase the concentration of the female sex hormone estrogen. This hormone causes the uterus to contract painfully during menstruation. This means that histamine can be partly responsible for menstrual problems such as menstrual pain.
Hormone fluctuations during pregnancy can have a positive effect on women with histamine intolerance: the histamine-related symptoms often disappear.
Histamine intolerance symptoms: Respiratory tract
During or immediately after eating histamine-rich meals or drinking alcohol, patients with histamine intolerance may develop symptoms such as a runny or stuffy nose. In extreme cases, an asthma attack with severe difficulty in breathing can also occur.
In patients with asthma, a certain enzyme often breaks down less histamine than in healthy people. As a result, histamine accumulates in the bronchial tubes independently of food intake. This can cause corresponding complaints.
Histamine intolerance: description and causes
With histamine intolerance (HI), the body reacts incompatibly to increased amounts of histamine. This so-called biogenic amine is formed in various cells such as mast cells, blood platelets and nerve cells from the protein building block (amino acid) histidine and then stored in these cells. Histamine can be released by certain stimuli, for example by the body’s own enzymes, various drugs and foods. Chemical stimuli in the context of inflammation as well as physical stimuli such as injuries or lack of oxygen can also stimulate histamine release.
As a biological messenger, histamine performs various functions in the body. For example, it stimulates the secretion of gastric juice, dilates the blood vessels and thus lowers blood pressure. As a nerve messenger (neurotransmitter), histamine regulates the sleep-wake rhythm, appetite control, learning ability, memory and emotions, among other things.
Above all, histamine acts as a mediator of inflammatory processes in allergic reactions: It triggers the typical allergy symptoms such as skin redness, wheals, itching, malaise, vomiting, diarrhoea, asthma attacks and headaches. These symptoms can also occur with histamine intolerance. Nevertheless, it is not a histamine allergy, which means that the HI symptoms are not triggered by an overreaction of the immune system to histamine.
Instead, experts suspect that an acquired or (more rarely) congenital disorder in histamine degradation triggers histamine intolerance. In the body of the affected person, more histamine is produced by the body’s own production and/or histamine-rich food than can be broken down. As soon as a certain limit value is exceeded, complaints arise. The level of this histamine limit is individually different.
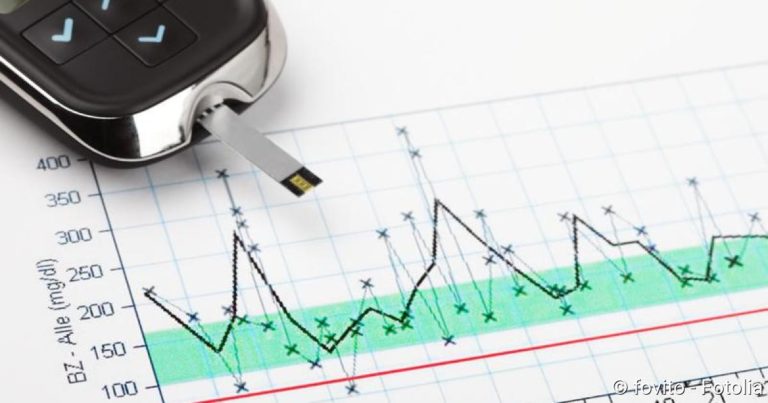
In case of a histamine intolerance the body cannot break down histamine sufficiently and the typical symptoms occur afterwards.
Disturbed histamine degradation
Basically the body has two different enzymes that can break down histamine:
- The enzyme histamine-N-methyl-transferase is located inside the cell and can therefore inactivate histamine in the cells.
- Diaminooxidase (DAO) is able to break down histamine, which is located outside the cells, for example in the blood.
The DAO is therefore largely responsible for the degradation of histamine from food. It therefore plays a central role in histamine intolerance: in some patients the enzyme may be present in insufficient quantities (enzyme deficiency). In others it may be reduced in its activity (disturbed enzyme function). Since DAO requires auxiliary substances such as vitamin B6 and vitamin C for histamine degradation, a deficiency of these vitamins can limit the function of the enzyme. However, there are also drugs that influence the activity of diaminooxidase (see below).
Whether enzyme deficiency or disturbed enzyme function – if the histamine turnover is out of balance, some people develop a histamine intolerance. In addition to histamine-rich foods and certain medications, increased endogenous histamine production can also trigger the symptoms of allergic diseases such as hay fever: The allergy-related increase in histamine in the body can exceed the enzymatic degradation capacity. This is especially true if the patient is also on a histamine-rich diet.
Histamine intolerance: the influence of drugs
Histamine is produced and stored in various cells as the body’s own messenger substance. Under certain stimuli it can be released from the cells and perform its functions. Such a stimulus can also emanate from some drugs, i.e. some drugs promote the release of histamine. Mostly this effect occurs as an undesired side effect.
In addition, certain drugs can influence the breakdown of histamine: Histamine from food is mainly broken down by the enzyme diaminooxidase (DAO). However, this enzyme is also responsible for the degradation of other metabolic products. If more of these products are produced by drug treatment, the enzyme can break down less histamine. As a result, the concentration of histamine increases.
Other drugs directly inhibit the function of diaminooxidase. This can also increase the histamine concentration and thus trigger complaints of histamine intolerance.
In the following, the most common drugs that can lead to an increased release or reduced degradation of histamine are listed. If the triggering drugs are discontinued again, in many cases histamine intolerance can be “cured” to a certain extent.
- all X-ray contrast media
- certain muscle relaxants (muscle relaxants such as suxamethonium)
- certain painkillers (acetylsalicylic acid, diclofenac, metamizole, morphine, etc.)
- Prilocaine (local anaesthetic)
- certain medicines for high blood pressure and heart diseases such as rhythm disturbances (dihydralazine, alprenolol, verapamil etc.)
- Furosemide (diuretic = diuretic)
- certain antibiotics (neomycin, vancomycin etc.)
- Metoclopramide (remedy for nausea and digestive disorders)
- certain mucolytics (acetylcysteine, ambroxol)
- certain medicines for asthma (aminophylline, theophylline)
- Amitryptilin (antidepressant)
- Cyclophosphamide (anti-cancer and anti-rheumatic agent)
- Cimetidine (remedy for heartburn and acid-related stomach problems)
Histamine intolerance: diet can trigger symptoms
Histamine and its precursor products are present in almost all foods and some beverages (see below: “Histamine intolerance: food”). However, the histamine content varies considerably and can be influenced by processing procedures such as maturation or fermentation. The consumption of histamine-rich foods increases the concentration of histamine in the body. If the histamine degradation cannot be increased accordingly, the histamine metabolism gets out of balance – symptoms may occur.
Histamine intolerance: associated diseases
In some inflammatory bowel diseases, a deficiency of the histamine-degrading enzyme diaminooxidase may occur. This means that less histamine can be broken down overall. This results in an increase in histamine concentration, which can cause symptoms of histamine intolerance.
In addition, there are other diseases that are associated with histaminosis. The enzyme diaminooxidase is also less active in them. These diseases include:
- Chronic renal failure
- virus-induced inflammation of the liver (viral hepatitis)
- Cirrhosis of the liver
- Hives (Urticaria)
- Seasickness
Histamine intolerance: a controversial disease
Histamine intolerance is a very controversial clinical picture: firstly, because the symptoms can vary considerably from patient to patient. Secondly, because the various symptoms can also occur in many other diseases. Diagnostics also often do not provide clear evidence of histaminosis. Some doctors therefore reject the clinical picture of histamine intolerance. Others, however, are convinced that it exists.
Experts assume that about one percent of the population suffers from a histamine intolerance. 80 percent of those affected are women. The middle age is considered the most frequent start of the disease with histamine intolerance.
Histamine intolerance: examinations and diagnosis
Many patients with a histamine intolerance have already had many visits to the doctor in which a cause for their complaints could never be found. Often the symptoms are unspecific and examination results do not reveal any pathological findings. A doctor usually only makes a histamine intolerance diagnosis if he has this clinical picture in mind. Targeted questions or a histamine intolerance test substantiate the assumption afterwards.
Doctor-patient consultation
The right contact person in case of suspected histamine intolerance is a specialist for skin diseases (dermatologist) or internal medicine (internist), who is specialized in allergic diseases (allergist). First of all, he takes your medical history (anamnesis). For this purpose, he will ask you about your current complaints and any previous illnesses, for example. Possible questions are, for example:
- Do you suffer from allergic diseases or food intolerances?
- Have you discovered a connection between your symptoms and the consumption of certain foods or do you keep a dietary diary?
- Will the symptoms improve if you avoid these foods?
- Are you taking medication regularly or as needed?
- With women: Are your symptoms related to your cycle?
Exclusion of other causes
The symptoms that occur with a histamine intolerance can also have other causes (differential diagnosis). For example, if you often have stomach aches and perhaps diarrhoea after eating, you may suffer from food intolerance (such as lactose intolerance, fructose intolerance, coeliac disease). A chronic inflammatory bowel disease such as Crohn’s disease or ulcerative colitis may also be behind it. Nausea and vomiting at the same time as a meal can also occur with an ulcer of the stomach lining (gastric ulcer). A reddened face with a feeling of heat (flush) can be the sign of a neuroendocrine tumor.
If histamine intolerance is suspected, the doctor must rule out such differential diagnoses. Which examinations are necessary depends on the symptoms. A stomach ulcer, for example, can be reliably detected or ruled out with a gastroscopy.
Histamine intolerance: test by means of a change in diet
With the help of a food test one can determine a possible histamine intolerance. At the same time, the individually tolerated histamine dose for each patient can be estimated.
This histamine intolerance test by means of a change in diet consists of three phases: the waiting period, the test phase and the permanent feeding. In all phases, in addition to nutrition, individual factors influencing histamine levels such as stress, the intake of certain medications and hormone status (menstruation) are taken into account.
Maternity leave: In this first phase of the dietary change, the symptoms that have occurred should be reduced as far as possible. For this purpose, the patient should not ingest histamine with food for 10 to 14 days. A completely histamine-free diet is hardly possible because histamine is contained in a great many foods. However, a special food list helps the patient to arrange his or her diet in such a way that he or she consumes as little histamine as possible.
In addition, the diet should also contain as few other biogenic amines as possible. These are also broken down by the histamine-degrading enzyme diamine oxidase (DAO). In larger quantities, they can therefore “employ” the enzyme in such a way that even small amounts of histamine can no longer be degraded. In addition, some biogenic amines can have a histamine-like effect (dilation of blood vessels) – another reason to keep their proportion in the diet low in the provocation test.
Test phase: This second test phase lasts up to six weeks. During this time, targeted “suspicious” foods are slowly reintroduced into the diet. Starting with a small amount of histamine, the histamine content of the food is gradually increased. At the same time, the patient writes down in a dietary diary which foods he or she has eaten on each day and whether any complaints have occurred. In this way, it is possible to estimate the individual histamine threshold at which signs of disease appear.
Permanent phase: From the findings of the test phase, the doctor can derive individual nutritional recommendations for the patient. These are suitable for a permanent diet. In making his recommendations, the physician takes into account not only the individually tolerated amount of histamine, but also the patient’s energy requirements and influencing factors such as hormone levels, medication intake or stress.
Histamine intolerance test: Provocation
With the dietary change described above, it is possible to estimate how much histamine someone can tolerate. This is often enough to ensure that the diet is appropriate in the future. If one wants to know exactly from which amount on someone develops histamine intolerance symptoms, one can carry out a “titrated provocation”. For this provocation test, the patient should first eat a diet as histamine-free as possible for some time and currently have no symptoms. The doctor then gives him increasing amounts of histamine (for ingestion) at two-hour intervals. The dose at which histamine intolerance symptoms occur is then considered the individual threshold dose.
The provocation test must be performed under medical supervision. If severe intolerance reactions such as nausea and vomiting up to temporary circulatory disorders occur, the doctor can treat them quickly.
Further histamine intolerance tests
Often other histamine intolerance tests are recommended to reliably detect histamine intolerance. However, the significance of such investigations is limited. They are among them:
- Measurement of DAO activity in blood serum: A possible cause of histamine intolerance (HI) is a reduced activity of the histamine-degrading enzyme diaminooxidase (DAO). Therefore, the DAO activity in the blood serum of the affected patients should be measurably reduced. According to experts, however, this procedure is not sufficiently meaningful to make a histamine intolerance diagnosis.
- Measurement of the amount of histamine in blood plasma: It is also said to be suitable as a histamine intolerance test. However, the validity of this study is controversial among experts. Besides histaminosis, conspicuous measured values can also have many other causes.
- Measurement of the amount of histamine in stool: Sometimes a histamine determination in stool is offered to clarify the suspicion of a histamine intolerance. However, various intestinal bacteria excrete large amounts of histamine. The measured values in the stool are therefore not very meaningful.
- Measurement of the amount of methylhistamine in urine: Methylhistamine is a breakdown product of histamine. Its concentration in urine is supposed to give indications of a possible histamine intolerance. However, this measured value generally depends on the protein content of the food. Therefore, the determination of methylhistamine as a histamine intolerance test is controversial.
- Histamine 50 prick test: The prick test is a widely used allergy test. The suspected irritant – in this case histamine – is injected into the patient’s skin in dissolved form (as drops). In case of intolerance, the skin reacts by forming wheals (skin blisters). If these are still present unchanged after 50 minutes, it is assumed that the breakdown of histamine in the skin is disturbed. However, this does not mean that the body cannot properly break down histamine ingested through food. Therefore, this histamine intolerance test is also viewed critically by experts.
Conclusion
None of the currently available histamine intolerance tests can reliably prove whether someone actually cannot tolerate externally supplied histamine (above a certain amount) and therefore reacts with complaints. Experts therefore recommend the following diagnostic steps to physicians if histamine intolerance is suspected:
- Collection of the medical history in the doctor-patient conversation (anamnesis)
- Examinations to exclude other possible causes for the complaints such as gastrointestinal ulcer (in case of nausea/vomiting) or lactose intolerance or fructose intolerance (in case of stomach ache, diarrhoea)
- Histamine intolerance test by means of a three-step dietary change
- If the change in diet has actually improved the symptoms, a titrated provocation test may be carried out to determine the individual histamine tolerance more precisely
Histamine intolerance: treatment
Histamine intolerance therapy mainly consists of avoiding triggering factors. This can be achieved above all with an appropriate diet. If possible, patients should also avoid medication that can trigger the symptoms of histamine intolerance. In certain cases, the use of certain drugs can help with histamine intolerance symptoms (drug-based histamine intolerance therapy).
Nutrition for histamine intolerance
Foods with a high histamine content such as old cheese or salted foods should not be consumed. In addition, people with histamine intolerance should avoid foods that can release histamine from the cell stores (histamine liberators such as tomatoes or strawberries). Also unfavourable are foods that contain larger amounts of other biogenic amines (bananas, pineapples, peanuts, etc.).
Furthermore, with a histamine intolerance diet, caution is also required when choosing beverages: Especially red wine is unfavorable for histamine intolerance. Coffee, on the other hand, is usually well tolerated in small quantities of one or two cups a day.
Tip: You can read more about unfavorable foods in case of histaminosis in the section Histamine intolerance: foods below.
How strictly those affected have to adhere to a histamine intolerance diet can be determined or tested in the course of diagnostics (three-stage dietary change, possibly provocation test). Don’t forget: The occurrence of symptoms depends on the total amount of histamine in the body – i.e. the histamine supplied with food plus the histamine produced in the body. However, individual histamine tolerance is not the same every day. It is influenced by various factors such as the interval between meals, alcohol consumption, medication, intestinal diseases or hormone status (menstruation). This means that despite a consistent low-histamine diet, a patient may be symptom-free one day and have symptoms such as wheals, itching and headaches the next.
Histamine intolerance: discontinue or change medication
Many drugs can trigger or worsen a histamine intolerance. Patients should therefore discontinue such preparations if the treating physician considers this to be justifiable. He may be able to recommend another drug that is better tolerated as an alternative.
Never discontinue medication on your own initiative, but always in consultation with the doctor treating you!
Drug-induced histamine intolerance therapy
Sometimes it is not possible to do without “critical” drugs. This can be the case, for example, with X-ray contrast agents used during examinations or muscle relaxants during operations. Patients with histamine intolerance can then receive antihistamines (histamine receptor blockers) as a preventive measure. These drugs block the docking sites of histamine (histamine receptors). Thus, despite the increased accumulation of histamine in the body, no or at least significantly fewer intolerance symptoms are triggered.
Antihistamines can also help with existing histamine intolerance symptoms.
Sometimes doctors use so-called mast cell stabilizers for histamine intolerance. Like antihistamines, they are actually used for allergies. Their effect is based on the fact that they stabilize the cell membrane of mast cells. As a result, they release less histamine (and other inflammatory messengers).
If there is a deficiency of the histamine-degrading enzyme diaminooxidase (DAO), it can be taken in capsule form. Such DAO preparations are available over the counter as dietary supplements. They can be taken before a meal if it contains a lot of histamine or if the histamine content cannot be estimated (e.g. when travelling or at family gatherings). If symptoms are already present, the enzyme preparation will no longer help.
The preparations mentioned for the prevention or alleviation of histamine intolerance symptoms are not a long-term substitute for a low-histamine diet. They serve only as a supplement and should be taken only as needed! Patient and doctor should discuss together whether and which preparations are useful. Some of the drugs (such as antihistamines) are also available only on prescription.
Vitamin preparations
Vitamin C and vitamin B6 are considered to be cofactors of diaminooxidase (DAO), which means that both vitamins are important for the function of the enzyme. Therefore, the intake of appropriate vitamin preparations can be useful. Patients should discuss this with their attending physician. If necessary, he can recommend a suitable preparation and dosage.
Histamine intolerance: food
Foods that contain a lot of histamine and/or other biogenic amines should be avoided in case of histamine intolerance. Also unfavourable are products that stimulate the release of histamine from its storage cells. Patients should therefore be familiar with these three food groups:
Histamine intolerance: Food with a lot of histamine
Histamine or its precursor histidine is found in almost all foods. However, the respective histamine content differs significantly. It is increased by maturing, fermentation and fermentation processes. Old Gauda, for example, contains more histamine than young Gouda, smoked ham more than cooked. Many bacteria or yeasts are capable of releasing histidine. High histamine concentrations are therefore not uncommon in microbially produced foods such as long-ripened cheese, wine or sauerkraut.
In addition, many people with histamine intolerance tolerate foods such as fish, meat and sausages poorly or not at all – because microorganisms often accumulate in these products. Last but not least, some vegetables naturally contain histamine, even when fresh – so they are also unfavourable for histamine intolerance.
A list of foods particularly rich in histamine can be found here:
- Fish: mackerel, herring, sardine, tuna
- Cheeses: Gouda, Camembert, Cheddar, Emmental, Swisstaler, Parmesan
- Meat: Sausage, salami, smoked ham
- Vegetables: sauerkraut, spinach, eggplant, tomatoes, avocado
- Alcohol: red wine, white wine, top and bottom fermented beer, champagne
- Other: red wine vinegar, soy sauce, yeast preparations
Histamine intolerance: Food with other biogenic amines
Besides histamine, other biogenic amines (such as tyramine, serotonin, spermine, cadaverine) are also degraded by the enzyme diamine oxidase (DAO). They may “employ” the enzyme so much that even small amounts of histamine can then no longer be degraded. Histamine overload can be the result. Some biogenic amines also have similar properties to histamine. They can therefore also directly trigger histamine-like symptoms.
Abundant biogenic amines contain, for example:
- Pineapple, bananas, papaya, pears, raspberries, oranges, kiwi
- Peanuts
- Pulses (lentils, beans, soya)
- Wheat germs
Histamine intolerance: foods that release histamine
So-called histamine liberators contain neither histamine nor other biogenic amines in large quantities. However, they can still trigger the symptoms of histamine intolerance. The reason: they ensure that the body’s own histamine is released from certain storage cells in the body (mast cells). Therefore, they should also be avoided in case of histamine intolerance. Among the histamine liberators are:
- Citrus fruits, strawberries
- Tomatoes, tomato puree, ketchup, tomato juice
- Chocolate, cocoa
- Seafood (mussels, crab)
- Nuts (especially walnuts and cashew nuts)
- Alcohol and its decomposition product acetylaldehyde
Nutritional tips for histamine intolerance
In case of histamine intolerance, foods of the critical groups mentioned above should be added to your diet as rarely as possible. Those who do not want to do without it completely should always distribute critical foods over several meals. For example, eating a slice of ripe Gouda in the morning and a small tomato as an afternoon snack is usually better tolerated than eating both histamine-rich foods at the same time.
In general, you should eat food as fresh as possible. Especially perishable dishes such as minced meat and fish should not be reheated a second time – eating them quickly leads to symptoms of histamine intolerance.
Here are some tips for certain foods and beverages:
Cheese: Avoid hard cheeses (such as Emmental, mountain cheese, Parmesan), long matured semi-hard cheeses (such as old Gouda), very mature mould cheeses (such as very soft Camembert) as well as raw milk and processed cheese. It is better to resort to young cheeses (such as butter cheese), spread cheese, cream cheese, cottage cheese and curd.
Sausage and meat: Instead of raw sausage (such as salami, raw ham, teewurst) you should choose cooked sausage (meat sausage, cooked ham). In the case of meat, particularly marinated (grilled meat, gyros, doner meat) and long-cooked meat (goulash, roast) are foods that often cause problems for people with histamine intolerance.
Fish: Avoid fish such as mackerel, anchovy, herring and tuna. Fresh or frozen fish is more digestible than smoked, dried and salted fish.
Alcohol: Red wine usually contains more histamine than white wine. French red wine, Chianti and nutmeg wine are particularly rich in histamines.
Candy and munchies: Chocolate and other sweets containing cocoa are usually poorly tolerated. The same sometimes applies to liquorice. Satisfy your desire for sweets better with fruit gums and sweets (both without azo dyes) as well as chocolate-free cakes and pastries. Salt sticks and potato chips without flavour enhancers and yeast extract are usually unproblematic in cases of histamine intolerance. Foods containing nuts (such as nut cakes), on the other hand, should be avoided, as they can release histamine.
Histamine intolerance: course and prognosis
The correct diet for histamine intolerance is the most important part of the treatment. Those who (largely) avoid histamine-rich foods can usually significantly improve their complaints. If certain drugs contribute to the histamine intolerance symptoms, the doctor can in many cases change the patient to a better tolerated preparation. In addition, if necessary, drugs such as antihistamine can alleviate the symptoms.
Many patients with histamine intolerance also suffer from food intolerances such as fructose, lactose or sorbitol intolerance. If too many foods (histamine-containing foods, fruit, dairy products, etc.) are removed from the diet, there may be a shortage. The diet for histamine intolerance plus food intolerances must therefore be planned particularly carefully. A nutritionist can give patients valuable support here.