Rosacea: symptoms, treatment, care
Rosacea: symptoms, treatment, care
Rosacea (rosacea) is an inflammatory, chronic disease of the facial skin that occurs in relapses. It begins with redness of the skin. Later, vasodilatation, vesicles, nodules and tissue neoplasms may be added. Those affected suffer from itching and pain, and the cosmetic impairment is also a burden. Here you can find out everything important about rosacea – symptoms, causes, diagnosis, treatment and prognosis.

Brief overview
- What is rosacea? Chronic inflammatory skin disease that progresses in phases and of varying severity. Mostly the face is affected, rarely also other parts of the body.
- Symptoms: Initially volatile reddening of the skin (erythema), later often vascular dilatation, inflammatory blisters and nodules as well as new tissue formation (phymas). Also burning, itchy skin and stinging pain. The special form of ophthalmorosacea affects the eye and can lead to severe visual impairment if left untreated.
- Triggers and risk factors:strong, long-lasting UV radiation (sunbathing, solarium), heat, hot baths and showers, certain cosmetics, washing lotions with alkaline pH values (>7), certain drugs, coffee and tea, alcohol and nicotine, stress.
- Treatment:medication (ointments, creams, lotions, antibiotics), laser treatment, obliteration, photodynamic therapy, surgical intervention; avoidance of typical triggers such as UV radiation, heat, spicy food, alcohol and certain care products and cosmetics
- Causes:Still unclear. A genetic predisposition in interaction with various immunological, microbacterial and neurological factors is suspected.
- Prognosis:Chronic course, not completely curable. With the right treatment, care and lifestyle, the symptoms can be well controlled and the relapses reduced. Sometimes the disease suddenly comes to a standstill.
Rosacea: Symptoms
Rosacea (rosacea, “copper rose”) is a disease of the skin (dermatosis). It classically affects the face and only rarely other parts of the body.
Rosacea progresses in phases and of varying severity, accompanied by typical symptoms. In addition, the symptoms can vary from patient to patient, so that they cannot always be clearly assigned to a severity level.
Preliminary stage: rosacea diathesis
Typical for the onset of rosacea are sudden, fleeting reddening of the skin (erythema). They mainly affect the cheeks, nose, chin and the middle forehead area. Rosacea rarely appears in other parts of the body such as the eyes, scalp, chest or neck.
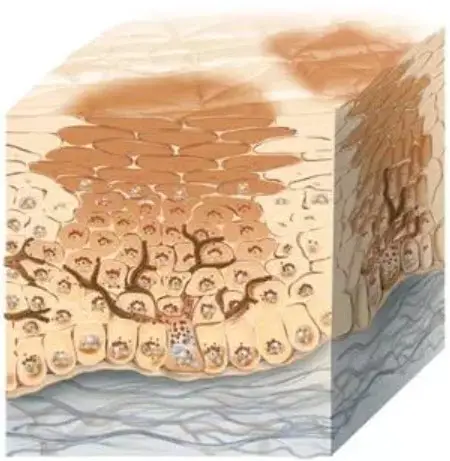
Severity I: Rosacea erythematosa-teleangiectatica
In addition to the reddening of the skin, vascular dilatations (telangiectasia) in the facial skin are also present. The skin is dry and occasionally flakes slightly. In addition, those affected suffer from itching and burning, stabbing pain.
Severity II: Rosacea papulopustulosa
In this stage form, additional inflammatory reddened blisters (pustules) and nodules (papules) appear as rosacea symptoms. They usually disappear only after several weeks. Sometimes lymphedema (accumulation of fluid) also develops in the facial tissue.
Because rosacea develops acne-like inflammatory skin changes, the disease was formerly mistakenly called “acne rosacea”.
Severity III: Glandular hyperplastic rosacea
This is the most severe form of rosacea. Connective tissue and sebaceous glands enlarge, resulting in bulbous growths (phymas), for example a bulbous nose or potato nose (rhinophyma). For cosmetic reasons, those affected usually suffer greatly from these skin changes.
Unlike acne, rosacea does not cause blackheads. If you are experiencing typical rosacea symptoms and blackheads at the same time, you are probably suffering from a mixed form.
Special forms of rosacea
In addition to classic rosacea, there are some special forms that occur relatively rarely.
Ophthalmorosacea is observed in about one in five people affected. It affects the eye, either in addition to the classic skin disease rosacea or in isolation. Typical symptoms are dilated blood vessels in the eyes as well as inflammation of the eyelids (eyelid inflammation = blepharitis) and conjunctiva (conjunctivitis). The eyes are also usually dry and often burn. Ophthalmorosacea should be monitored particularly closely. Untreated, it can cause corneal inflammation (keratitis), which in extreme cases can lead to blindness.
In rosacea fulminans, the typical symptoms become particularly pronounced within a few days or weeks. It is mainly young women who are affected, whereas men are hardly ever affected. Once rosacea fulminans has been overcome, it usually does not recur.
Gram-negative rosacea occurs when the disease has been treated with antibiotics for several weeks without lasting success. Then only certain pathogens were destroyed. Others, so-called gram-negative bacteria, have survived. They multiply and subsequently cause further skin reactions.
If rosacea is treated with glucocorticoids (steroid hormones such as cortisone), steroid rosacea may develop after discontinuation of the medication. This is often much more severe than rosacea, which was actually intended to be treated. For this reason, rosacea is only treated with these drugs in exceptional cases.
The inflammatory skin disease rosacea is mainly manifested by severe redness of the face. With a special form, the eyes can fall ill and be damaged.
Rosacea: treatment
With special medication and the right cosmetic care, rosacea symptoms can often be significantly alleviated. If left untreated, rosacea usually worsens in phases.
In addition or as an alternative to drug treatment, other therapeutic methods can be used. These include obliteration, photodynamic therapy and surgical procedures. In addition, people with rosacea should keep an eye on their diet and avoid typical triggers of the symptoms as far as possible.
Some patients use homeopathy in the treatment of rosacea (often in addition to conventional medical therapy). An effectiveness of the alternative healing method has not yet been scientifically proven. Nevertheless, some patients report an improvement of the symptoms.
Rosacea treatment with medication
Drug treatment is the most important component of rosacea therapy. A distinction is made here between local and systemic therapy. Experience shows that the combination of local and systemic rosacea therapy is particularly effective.
Local (topical) rosacea treatment
Here, the medication is applied as an ointment, gel or lotion directly to the affected skin areas. Which dosage form is most effective and best tolerated depends on the individual case. External treatment of rosacea is usually carried out over a very long period of time (as topical maintenance therapy). The two main active ingredients used in this process are:
Both agents are believed to have an anti-inflammatory effect in rosacea. They may also slow down the immune system, which typically overreacts in rosacea. Azelaic acid also ensures that certain skin cells (keratocytes) do not grow too much.
In addition, other substances can be used for local rosacea therapy:
- Permethrin: Correctly dosed, the actual toxin has a positive effect on rosacea.
- Clindamycin: The antibiotic is also used locally in exceptional cases.
- Retinoids: Like permethrin, they are also used for acne.
- Calcineurin inhibitors: They are particularly helpful in steroid rosacea.
The above-mentioned active ingredients primarily combat the nodules and blisters. However, they usually do not help against the typical reddening of the face. In contrast, a special gel with the active ingredient brimonidine was developed in the USA. Since 2014 it has also been approved in the EU. The drug causes the blood vessels in the facial skin to contract. This causes the redness to fade.
Systemic rosacea treatment
For some milder forms of rosacea, local treatment is sufficient. In more severe cases, however, systemic rosacea treatment is also necessary. The drug is used internally, for example in the form of tablets. In this way, the active ingredient reaches the entire body via the blood. This makes systemic rosacea therapy more effective than local therapy. On the other hand, there are often more severe side effects.
Most commonly, antibiotics are used for systemic rosacea therapy, especially two groups:
- Tetracycline: Doxycycline and minocycline are the most commonly used drugs in this group of active ingredients. They are the first choice for antibiotic treatment of rosacea because they are better tolerated by the stomach and intestines than macrolides.
- Macrolides: Erythromycin and clarithromycin, for example, belong to this group of active ingredients. Macrolides are used when patients cannot tolerate tetracyclines.
Antibiotics are actually used to fight bacteria. In rosacea treatment, however, a different mechanism of action of these substances is used: In low doses, the antibiotics have a predominantly anti-inflammatory and attenuating effect on the overreacting immune system – similar to metronidazole and azelaic acid in local rosacea treatment.
In addition to antibiotics, systemic rosacea is sometimes treated with agents that are normally used for local treatment – for example, tablets containing metronidazole.
Retinoids such as isotretinoin can also relieve rosacea symptoms when used internally, as studies show. However, isotretinoin is only approved in Germany for the treatment of severe acne. It is therefore only used in severe rosacea in exceptional cases outside the official approval (“off label”). Great caution is required, because taking isotretinoin capsules can have many side effects (even severe ones), for example irritation of the skin and mucous membranes. In addition, isotretinoin must not be taken by women who could become pregnant (risk of fetal malformations!).
Unlike many other skin diseases, rosacea is only treated with glucocorticoids (“cortiosn”) in exceptional cases, as these drugs usually worsen the clinical picture. Even after an initial improvement, the symptoms usually return all the stronger after discontinuing the cortisone preparation.
Laser treatment and obliteration
With laser treatment, the persistent redness and vascular dilatation (telangiectasia) can usually be eliminated well. For this purpose, the affected skin areas are treated with bundled, high-energy light rays. In this way also phymas can be removed.
Vasodilatation can also become deserted with the help of electric current.
Photodynamic therapy (PDT)
In photodynamic therapy, rosacea patients first receive a substance that makes the skin more light-sensitive. This so-called photosensitizer accumulates on the affected skin areas. Then these areas are irradiated with light of a certain wavelength. This changes the structure of the photosensitizer. As a result, the substance destroys defective skin structures.
Surgical therapy
Rosacea can also be treated surgically, for example with dermabrasion or dermashaving. These methods are mainly used for phymas. They are therefore described in more detail in the article “Rosacea: Rhinophym”.
Change your diet & avoid triggers
It is also very helpful when people with rosacea change their diet. Although there is no special rosacea diet. However, since experience has shown that hot spices, very hot food and drinks and alcohol can lead to vasodilatation in the face, it is better for the patient to avoid this. Ensure a healthy, balanced diet. In particular, reduce your fat and sugar consumption in favour of lots of fruit and vegetables. This way you can prevent the pores of the facial skin from clogging. This in turn has a positive effect on the skin’s appearance.
You should also test how your rosacea reacts to different foods. To do this, consciously avoid certain foods and observe whether and how the rosacea symptoms change as a result.
It is also important that you avoid the typical triggers of a rosacea relapse:
- strong, long-lasting UV radiation (sunbathing, solarium)
- Heat, hot baths and showers, sauna visits
- Washing lotions and soaps with alkaline pH value (>7)
- certain cosmetics
- certain drugs
- Coffee and tea
- Alcohol
- Nicotine
- Stress
Hormonal changes, for example during pregnancy, can also trigger a flare-up of the disease. Talk to your doctor about this.
Rosacea patients react differently to the various possible triggers. Therefore, observe closely to which stimuli your skin reacts and adjust your lifestyle accordingly.
Rosacea: Care
Rosacea skin should be properly cared for. This can support treatment with medication and/or other therapeutic methods. This is because certain ingredients and improper use of care products can irritate the skin and thus aggravate the symptoms.
Correct skin care
Follow these tips for skin care:
- Clean the skin of your face with lukewarm water only. Extreme water temperatures and rapidly successive temperature changes can lead to sudden reddening of the skin (flush).
- Do not use facial peelings, as they additionally irritate the rosacea skin.
- Only use care and washing products without menthol, camphor, sodium lauryl sulphate and astringents.
- Avoid water with a high degree of hardness.
- After washing, gently pat the skin of the face dry with a towel instead of rubbing it with the towel.
- Use soaps and washing lotions with a slightly acidic pH value (< 7).
As far as facial cleansing is concerned, so-called washing syndets are well suited for rosacea patients. These are artificial washing-active substances with a relatively low pH value (4.5 to 5.5) which are much gentler to the skin than classic soaps.
The fine vessels of the skin dilate: The skin of the cheeks reddens because the smallest blood vessels dilate (telangiectasia) – the veins are clearly visible.
Be careful with the sunlight!
UV rays are an important risk factor for rosacea sufferers. Therefore you should conscientiously protect your skin from (strong) UV radiation:
- Avoid direct sunlight between spring and autumn.
- Do not visit a solarium.
- Use sun protection products with a high sun protection factor (50+) and apply them several times a day. Prefer physical sunblockers with titanium dioxide or zinc oxide (pharmacy). In rosacea, these are considered to be better tolerated by the skin than chemical sunscreens.
Rosacea: cream, ointment or lotion?
The products differ in terms of water and fat content. An ointment contains no water at all, only fat. In contrast, a cream has a certain amount of water. A lotion even contains more water than fat. It is therefore also called an oil-in-water emulsion.
For rosacea patients, products with a high water content are ideal, i.e. creams and lotions. This is because they do not form a greasy film on the skin that closes pores, but allow the skin to breathe without drying it out. The same applies to preparations based on glycerine or silicone oil (cyclomethicone, dimethicone).
You should avoid products with added fragrances or dyes completely, as they irritate the skin unnecessarily.
Tip: Before buying your care products, get detailed advice at the pharmacy.
Make-up for rosacea
Basically you can also use make-up with rosacea. However, you should make sure that the products are free of skin-irritating ingredients such as menthol, camphor, sodium lauryl sulfate and astringents. Moreover, the cosmetics should not clog the sebaceous glands, i.e. they should not be comedogenic.
Do not use very thick make-up. This is because it is difficult to remove, which in turn can cause skin irritation. A special rosacea make-up that covers the redness of the face well and can be easily removed is recommended.
Rosacea sufferers can react very individually to cosmetics. If you notice that you do not tolerate a product, you should stop using it immediately and try an alternative.
Rosacea: Rhinophyma
Rhinophyma is a symptom of rosacea that can develop during a severe course of the disease. This is a proliferation of the connective tissue and the sebaceous glands (phyme). Rhinophymes usually occur on the nose. This so-called tuber nose or potato nose is especially observed in older men.
Phyme is treated with medication or surgery. Especially in the surgical field, good optical treatment successes can be achieved today. However, there is a possibility that a new tuber nose may form later.
You can read more about the “rhinophym” in rosacea in the article Rosacea: Rhinophym.
Rosacea: causes and risk factors
Depending on which study is used as a basis, between 2 and 20 percent of the population in Germany suffer from rosacea. People over the age of 30 are most frequently affected. But even children can suffer from rosacea in exceptional cases. No significant differences between the sexes can be observed – rosacea occurs only minimally more frequently in women. In addition, light skin types are more frequently affected than dark ones.
The typical symptoms of rosacea are a permanent dilation of the blood vessels and chronic inflammation of the skin. The reasons for this are not yet fully understood. A genetic predisposition is suspected. In combination with various factors, it could lead to the development of rosacea, experts believe.
How does rosacea develop?
Among other things, the body’s own immune system probably plays a role. It produces certain antimicrobial substances in the skin that are designed to combat incoming pathogens. Some of these substances trigger inflammation and also cause new vessels to form (angioneogenesis). This is normal and useful for destroying invading pathogens. However, significantly elevated concentrations of these antimicrobial substances have been detected in the blood of rosacea patients. This could explain the pathological skin inflammation and tissue formation.
Certain microorganisms are suspected to be the trigger of the immune reaction. The skin of rosacea sufferers is often colonized to an above-average extent by so-called hair follicle mites (Demodex folliculorum). The microscopically small animals are indeed on the skin of every human being. In rosacea patients, however, they appear to be more common and to trigger the inflammatory immune response described above.
In addition, there is evidence that immune system receptors do not work properly in rosacea. These receptors recognise foreign organisms and produce certain substances to combat them. In case of a faulty regulation, however, the receptors overreact and thus trigger persistent skin inflammations.
Last but not least, inflamed nerves in the face also seem to play a role in the development of rosacea. The nerves control the blood vessels by making them dilate when hot and contract when cold. However, in rosacea patients, communication between nerves and blood vessels in the face does not function properly because the nerves are inflamed. This leads to malfunctions – even weak stimuli such as spicy food cause the blood vessels to dilate without contracting completely afterwards.
Rosacea: examinations and diagnosis
In most cases, the dermatologist can already recognize rosacea by its typical symptoms (reddening of the skin, dilated vessels, etc.). Special investigations are therefore generally not necessary.
However, sometimes the doctor will take a skin sample (biopsy) if rosacea is suspected. It is examined more closely under the microscope. Thus, visually similar skin diseases can be excluded, such as the rarer butterfly lichen or the stewardess disease (cosmetic acne). The examination also helps to assess the severity of rosacea.
Rosacea: course of the disease and prognosis
Rosacea is usually chronic and intermittent – periods of more severe symptoms alternate with periods when the symptoms subside or at least improve. Although the disease is not completely curable, it is easily controlled with proper treatment, skin care and lifestyle. Sometimes rosacea even comes to a standstill without developing further.