Myocarditis: symptoms, triggers, risks
Myocarditis (Heart muscle inflammation): symptoms, triggers, risks
Myocarditis (inflammation of the heart muscle) is a serious disease. It often develops as a result of flu-like infections. Their symptoms are often barely noticeable, which makes a quick diagnosis difficult. In severe cases, myocarditis can trigger cardiac insufficiency or severe cardiac arrhythmia. Then there is even the danger of sudden cardiac death. Here you can read about how you can recognise an inflammation of the heart muscle, how it develops and how it is treated.

Brief overview
- What is myocarditis? Inflammation of the heart muscle cells and usually also of the surrounding tissue and the blood vessels supplying the heart (coronary arteries). If the inflammation also spreads to the pericardium, this is called perimyocarditis.
- Symptoms: often no or hardly noticeable symptoms such as increased palpitations (palpitations) and heart stumbling; possibly chest pain, cardiac arrhythmia and signs of heart failure in advanced myocarditis (such as water retention in the lower legs)
- Triggers: In infectious myocarditis, pathogens such as viruses (e.g. cold, flu, herpes, measles or coxsackie viruses) or bacteria (e.g. the pathogens causing tonsillitis, scarlet fever, diphtheria or blood poisoning) are involved. Non-infectious myocarditis is caused by, for example, faulty immune reactions, radiotherapy or medication.
- Risks: Possible consequences are a pathologically enlarged heart muscle (dilated cardiomyopathy) with chronic cardiac insufficiency and severe cardiac arrhythmia. There is a risk of sudden cardiac death.
- Treatment: mainly physical rest and bed rest, possibly medication against the pathogens causing infectious myocarditis (such as antibiotics against bacteria); treatment of complications, e.g. heart-stressing medication for cardiac insufficiency (such as beta blockers)
- Prognosis: With consistent physical protection the myocarditis usually heals without consequences. Otherwise there is a risk of late effects such as heart failure. Rarely does heart muscle inflammation end fatally.
Myocarditis: Symptoms
Heart muscle inflammation (myocarditis) is usually caused by viruses or bacteria (infectious myocarditis). The symptoms of such an infection therefore often precede myocarditis. These can be, for example, a cold and cough, fever, headache and aching limbs. If these flu-like symptoms are accompanied by increasing tiredness and exhaustion, weakness, decreasing resilience or difficulty in breathing during exertion, the possibility of infectious myocarditis should always be considered.
In fact, these complaints are often the only signs at the beginning of an acute heart muscle inflammation. Symptoms such as appetite and weight loss as well as headaches and aching limbs can be added. Other myocarditis symptoms may include radiating pain in the neck or shoulders.
If you develop possible symptoms of heart muscle inflammation days or weeks after a flu-like infection, you should definitely see your doctor!
Heart symptoms
Normally a healthy person cannot feel his heart. However, in the case of myocarditis, some people notice increased heart palpitations. Some also report a feeling of tightness in the chest (atypical angina pectoris) or heart stumbling. This stumbling expresses the fact that the heart gets out of step for a short time every now and then:
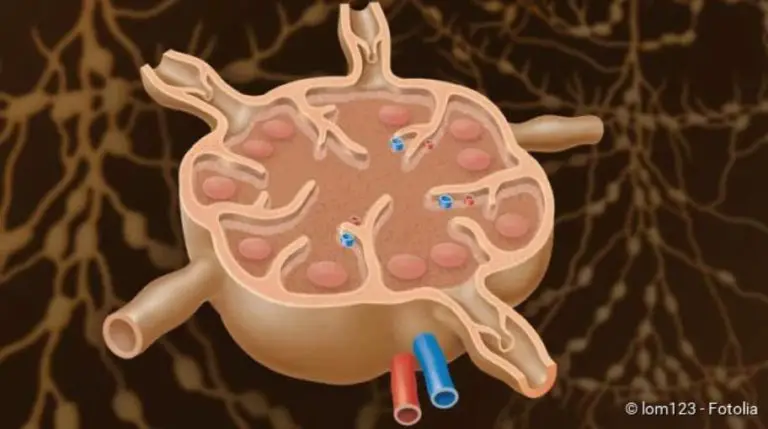
The heart has a clock that is located in the right atrium. From this so-called sinus node, in a healthy heart the electrical signals spread evenly across the heart muscle and trigger its contraction. The heart thus beats in a coordinated manner and pumps the blood evenly into the body’s circulation.
In the case of heart muscle inflammation, additional electrical signals are generated or their normal transmission is delayed. Sometimes the impulses are not even transmitted at all from the atrium to the chambers (AV block). The normal heart rhythm is therefore disturbed. In some cases of heart muscle inflammation, this leads to palpitations (tachycardia) or irregular heart rhythms with dropouts.
Myocarditis: Triggers & Causes
With regard to the causes, a distinction is made between infectious and non-infectious heart muscle inflammation.
The mostly painless myocarditis can weaken the heart muscle considerably and cause cardiac arrhythmia.
Infectious Myocarditis
A myocarditis is called infectious if it is caused by pathogens. In about 50 percent of cases, these are viruses. Infectious myocarditis is often preceded by a common viral infection (cold, flu, diarrhoea). Especially the so-called Coxsackie B virus is often the trigger for viral myocarditis. But many other viruses, such as the pathogens that cause herpes, flu (influenza), mumps, rubella or measles, can also cause heart muscle inflammation.
If viral myocarditis is suspected, the triggering virus is only determined in exceptional cases. This would be of little practical use – there are usually no specific drugs against the viruses in question.
Bacteria can also cause heart muscle inflammation. Particularly in the context of bacterial blood poisoning (sepsis), in which the heart valves are already affected, the inflammation can also spread to the heart muscle. Typical pathogens here are so-called staphylococci. Another group of bacteria, streptococci, can also cause heart muscle inflammation. These include, for example, the pathogens of scarlet fever or tonsillitis.
Another bacterial cause of myocarditis can be diphtheria. Lyme disease is rarely the cause of an inflamed heart muscle. Their pathogen, the bacterium Borrelia burgdorferi, is transmitted by a tick bite.
Fungal infections are also rarely the trigger of infectious heart muscle inflammation: fungi usually only trigger myocarditis when the patient’s immune system is significantly weakened. This is the case, for example, with AIDS, chemotherapy or the use of immunosuppressive drugs.
Other rare pathogens of heart muscle inflammation are parasites such as the fox tapeworm or unicellular organisms such as the pathogens of toxoplasmosis or Chagas’ disease.
Non-infectious heart muscle inflammation
In non-infectious myocarditis, no pathogens are the trigger. Instead, the cause is, for example, a defective regulation of the immune system. The immune system is directed against the body’s own structures, resulting in so-called autoimmune diseases. These include, for example, vascular inflammation, inflammation of connective tissue and rheumatic diseases. Such autoimmune diseases can also lead to heart muscle inflammation (autoimmune myocarditis).
Another cause of non-infectious heart muscle inflammation is irradiation of the chest as part of radiotherapy for various types of cancer (such as lung cancer).
Rarely do drugs trigger non-infectious myocarditis. These can be, for example, the antibiotics penicillin and ampicillin, the diuretic hydrochlorothiazide and the blood pressure reducer methyldopa.
If no trigger at all is found for the heart muscle inflammation, the doctor speaks of the so-called idiopathic fiddler’s myocarditis.
Myocarditis (Heart muscle inflammation): Risks
Heart muscle inflammation can be very dangerous – especially if the affected person does not take enough care of himself or has a damaged heart. Myocarditis can cause severe cardiac arrhythmia. These have considerable consequences for the circulation. Because the heart needs the calm, steady rhythm to fill up with blood after each heartbeat for the next powerful contraction. If it beats too quickly or irregularly due to myocarditis, it cannot fill or empty itself properly. Possible consequence is a circulatory collapse with sudden cardiac death.
In about one in six patients, myocarditis triggers remodelling processes in the heart, which ultimately lead to chronic cardiac insufficiency: The damaged heart muscle cells are converted into scar tissue (fibrosis), the heart cavities (ventricles, atria) dilate. Doctors speak of dilated cardiomyopathy. The walls of the pathologically enlarged heart muscle are “worn out” to a certain extent, so that they can no longer contract powerfully. So a permanent heart failure has developed. In severe cases, the pumping capacity of the heart can collapse completely. Sudden cardiac death can therefore also occur here.
Myocarditis (Heart muscle inflammation): examinations and diagnosis
If heart muscle inflammation is suspected, your family doctor or a cardiology specialist is the right person to contact. If necessary, the doctor will refer you to a hospital for further examinations.
Doctor-patient consultation
The doctor will first talk to you in detail to take your medical history (anamnesis). He will ask about the exact symptoms and whether they were possibly preceded by an infection (cold, flu, diarrhoea, etc.). The doctor will also ask whether you suffer from any underlying diseases (especially heart disease) or have already had heart surgery.
Physical examination
This is followed by a thorough physical examination. Among other things, the doctor will listen to your heart and lungs with a stethoscope, tap your chest and measure your pulse and blood pressure. He also checks to see if you show signs of incipient heart failure. These include, for example, water retention (edema) in the lower legs.
ECG (electrocardiography)
Another important examination is the measurement of the electrical activity of the heart muscle (electrocardiography, ECG). Changes in heart activity, such as those that occur during myocarditis, can be detected. Typical are an accelerated heartbeat (racing heart) and additional beats (extrasystoles). Heart rhythm disturbances are also possible. Since the deviations usually occur only temporarily, a long-term measurement of the heart activity (long-term ECG) is advisable – in addition to the usual short-term resting ECG.
Heart ultrasound
By means of an ultrasound examination of the heart (echocardiography) the doctor can assess the structure and function of the heart muscle. For example, he can detect enlarged ventricles or pumping weakness. In some heart muscle inflammations, fluid also collects between the pericardium and the heart muscle. Such a pericardial effusion can also be detected in ultrasound.
Blood test
Inflammation values in the blood (CRP, BSG, leukocytes) show whether there is an inflammation in the body. In addition, cardiac enzymes such as troponin-T or creatine kinase are also determined: They are released from the cells when heart muscle cells are damaged (for example as a result of myocarditis) and are then detectable in the blood in increased quantities.
If antibodies against certain viruses or bacteria are found in the blood, this indicates a corresponding infection. If the heart muscle inflammation is the result of an autoimmune reaction, corresponding autoantibodies (antibodies against the body’s own structures) can be detected.
X-ray
An X-ray of the chest (chest x-ray) can reveal signs of heart failure due to myocarditis. The heart is then enlarged. In addition, a backlog of fluid in the lungs may be visible, which is caused by the weak pumping power of the heart.
Magnetic resonance imaging (MRI)
Using magnetic resonance imaging (MRI), the physician can distinguish inflamed, damaged heart areas from healthy ones. An MRI of the heart is called a cardiac MRI.
Tissue removal by means of heart catheter
Sometimes an examination by means of a cardiac catheter is also carried out in the case of heart muscle inflammation. A small tissue sample of the heart muscle can be taken (myocardial biopsy). It is examined in the laboratory for inflammatory cells and pathogens.
Myocarditis: Treatment
The treatment of heart muscle inflammation depends on the symptoms on the one hand and on the trigger on the other. Physical protection and the treatment of a possible underlying disease are the cornerstones of myocarditis treatment.
In case of a very severe heart muscle inflammation, the patient must be treated in the intensive care unit. There, vital parameters such as heart activity, pulse, oxygen saturation and blood pressure can be continuously monitored.
Physical protection
It is particularly important in the case of heart muscle inflammation that the patient takes complete physical rest. This means that he must avoid any physical exertion, for example in the household. This is because heart muscle inflammation can leave lifelong damage to the heart muscle and heart valves if it is further fired by stress.
Patients with severe heart muscle inflammation are admitted to hospital.
Even weeks after the acute phase of the disease, the patient must not overexert himself. The doctor decides when full weight bearing is possible again. As long as there are signs of heart failure, the patient is unable to work. If he strains himself again prematurely, he risks a relapse and permanent damage.
If myocarditis requires prolonged bed rest, there is a risk of blood clots forming (thrombosis). Patients are given anticoagulants as a preventive measure.
Treatment of the cause
The most common pathogens of infectious heart muscle inflammation are viruses. However, there are usually no antiviral drugs available to treat such viral myocarditis. The treatment here essentially consists of rest and bed rest.
The situation is different with bacterial myocarditis: The doctor prescribes antibiotics against the bacteria that cause the disease. Targeted drugs can also usually be used against other pathogens that cause myocarditis in rare cases. These include antimycotics against fungal infections and antiprotozoals against unicellular parasites (such as the pathogens causing Chagas’ disease).
In certain cases, other therapies are also possible for myocarditis (in some cases only within the framework of studies). This could be the administration of cortisone. It has an anti-inflammatory effect and suppresses the immune system. This can be useful in myocarditis, where antibodies are formed against the body’s own structures (autoantibodies) due to a misregulation of the immune system.
Treatment of complications
A possible complication of heart muscle inflammation is heart failure. The doctor can then prescribe various drugs, for example ACE inhibitors, AT1 receptor antagonists or beta blockers. They relieve the weak heart. The same is also done by diuretic drugs.
Sometimes the heart beats so irregularly and rapidly in myocarditis that a life-threatening cardiac arrhythmia such as ventricular tachycardia or ventricular fibrillation is imminent. In this case, patients may be temporarily fitted with an external shock generator (defibrillator). In case of ventricular fibrillation, the device automatically emits a strong electrical impulse to restore normal heart rhythm. Fortunately, this measure is rarely necessary.
If fluid has accumulated in the pericardium during myocarditis (pericardial effusion), it should be aspirated with a thin, fine hollow needle (pericardial puncture).
In the worst case, myocarditis can damage the heart so severely and permanently that it can no longer maintain its function. Then the patient needs a donor heart (heart transplantation).
Myocarditis (Heart muscle inflammation): course of disease and prognosis
Myocarditis can occur at any age and can also affect young, heart-healthy people. If patients consistently take care of their bodies, the course of the disease and prognosis are usually good. Overall, heart muscle inflammation heals in more than 80 percent of cases without leaving any permanent damage. This is especially true in the case of viral myocarditis. In some patients, harmless extra beats of the heart can then be found in the ECG (electrocardiogram).
The problem with myocarditis is that it sometimes causes hardly any symptoms. Many patients therefore do not spare themselves sufficiently. This can be observed especially in young people who do sports despite myocarditis. The possible consequences include severe cardiac arrhythmia, which can lead to sudden cardiac death. However, this happens only rarely.
Myocarditis: Duration
An acute heart muscle inflammation lasts on average about six weeks. In individual cases, the duration of the disease depends on the extent of the inflammation and the patient’s general health.
It is also very difficult to say when a heart muscle inflammation has really healed completely. Even if an affected person feels completely healthy again after surviving myocarditis, he should take it easy for a few weeks and avoid physical exertion. This is the only way to avoid serious long-term consequences (such as heart failure).
Chronic heart muscle inflammation
In some patients the heart muscle inflammation is chronic. The heart muscle or the ventricle (especially on the left side) is dilated (dilated cardiomyopathy). The chamber walls are remarkably thin and can no longer provide the necessary pumping force. As a result, the heart is restricted in its function – a cardiac insufficiency (heart failure) has developed. Even slight exertion (such as climbing stairs) causes the affected person to experience shortness of breath (dyspnoea). Heart failure must usually be treated with medication.
Heart muscle inflammation: Prevention
Inflammation of the heart muscle can be prevented by vaccination against the infectious diseases that cause it and by having these vaccinations refreshed as prescribed. The recommendations of the Standing Commission on Immunization (STIKO) at the Robert Koch Institute should be followed. For example, vaccination against diphtheria is advisable. In addition to the risk of heart muscle inflammation, this bacterial infectious disease carries other dangers such as severe pneumonia. The vaccination is usually administered in childhood together with those against tetanus and polio.
It is also very important to cure flu-like infections properly. Physical exertion should be consistently avoided with every fever. The same applies even in the case of a seemingly harmless cold. If such an infection is “carried away”, the pathogens (viruses or bacteria) can easily spread to the heart and cause heart muscle inflammation.
People who have already had myocarditis once are particularly at risk of developing it again (relapse). You should therefore be particularly careful. Above all, the combination of physical strain, stress and alcohol should be avoided. In addition, bacterial skin and mucous membrane inflammations should be treated with antibiotics at an early stage. Such diseases are often the trigger for a new heart muscle inflammation.